It's strange that everyone on health policy twitter is not going apes over the Hospital Outpatient Prospective Payment System (#OPPS) rule released today
It contains one hugely significant proposal that hospitals will fight bitterly...but could actually help them in the long run
It contains one hugely significant proposal that hospitals will fight bitterly...but could actually help them in the long run
Background- there are two different CMS payment systems for historic/operational reasons, one for professional services, and the other for hospital outpatient depts.
Up until now, there had never been an effort to make sure that equivalent services would have same payment rate.
Up until now, there had never been an effort to make sure that equivalent services would have same payment rate.
In fact, the same procedure paid for in hospital OPD setting ended up being reimbursed at a much higher rate than the exact same procedure at a doctor’s office.
Here’s how @MartinSGaynor and Paul Ginsburg and I described it in our “Making Markets Work” White Paper
Here’s how @MartinSGaynor and Paul Ginsburg and I described it in our “Making Markets Work” White Paper
It was natural that, responding to these incentives, hospitals began buying up physician practices and rebadging them as “hospital outpatient departments”
Private cardiologists could not compete with this arbitraged employment arrangement, and Medicare’s payments skyrocketed
Private cardiologists could not compete with this arbitraged employment arrangement, and Medicare’s payments skyrocketed
what’s worse is that Medicare beneficiaries began to get surprise bills for separate hospital fees when they thought had already paid their copay for their doctor’s visit.
there are 100’s of local news stories about this like this one
nbcconnecticut.com/investigations…
@RosenthalHealth
there are 100’s of local news stories about this like this one
nbcconnecticut.com/investigations…
@RosenthalHealth
Policy experts including the @medicarepayment advised government to eliminate these facility fees and enact “site-neutral payments” saving hundreds of millions of dollars, and slowing down hospital consolidation.
@JohnArnoldFndtn
modernhealthcare.com/article/201306…
@JohnArnoldFndtn
modernhealthcare.com/article/201306…
Congress in 2015 as part of the Bipartisan Budget Act stopped any *new* sites from being converted from private practices to “hospital outpatient departments", but grandfathered the old ones, and left open the door to lots of games.
@rshawnm @aafpprez
aafp.org/news/governmen…
@rshawnm @aafpprez
aafp.org/news/governmen…
I have to give credit to the current Administration for taking seriously the growing threat to markets of hospital consolidation.
The 2018 president’s budget proposed eliminating grandfathered, “mid-build", emergency departments & cancer hospital exceptions to site-neutral pay
The 2018 president’s budget proposed eliminating grandfathered, “mid-build", emergency departments & cancer hospital exceptions to site-neutral pay
…which brings us to today.
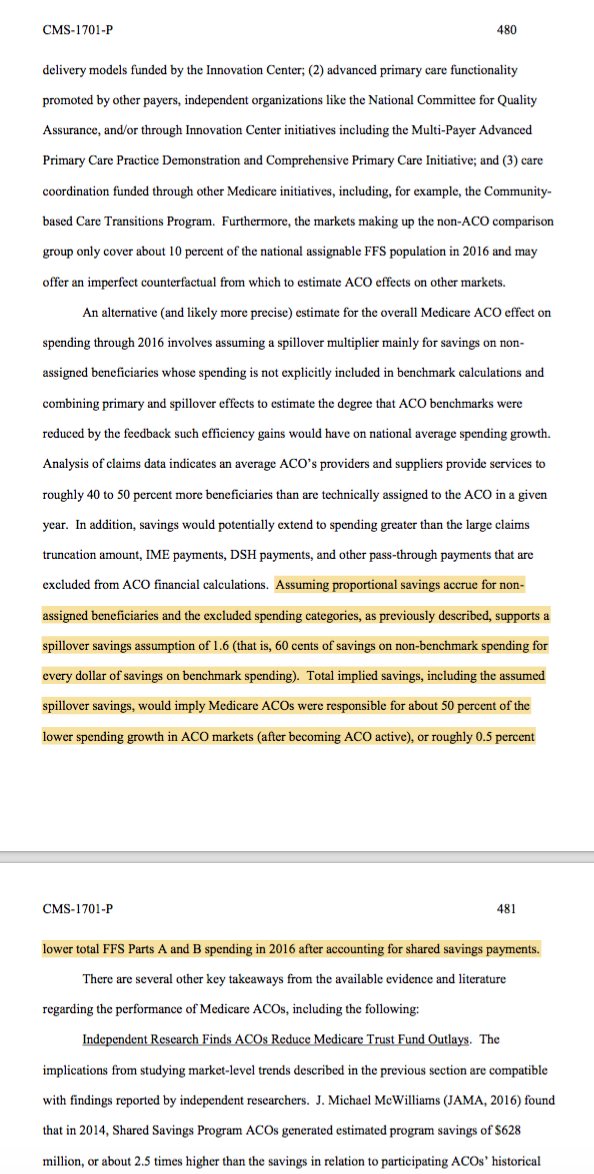
The annual hospital OPPS payment rule proposes to cap the OPPS payment at the Physician Fee Schedule (PFS)-equivalent rate for the office visit (G0463) and seeks to expand to additional items and services and freezes services in grandfathered sites
The annual hospital OPPS payment rule proposes to cap the OPPS payment at the Physician Fee Schedule (PFS)-equivalent rate for the office visit (G0463) and seeks to expand to additional items and services and freezes services in grandfathered sites

They will be sued
The legal argument:
Section 4523 of the BBA of 1997 (established OPPS) Included specific authority under section 1833(t)(2)(F) of the Act that requires the Secretary to develop a method for controlling unnecessary increases in the volume of covered OPD services
The legal argument:
Section 4523 of the BBA of 1997 (established OPPS) Included specific authority under section 1833(t)(2)(F) of the Act that requires the Secretary to develop a method for controlling unnecessary increases in the volume of covered OPD services
This will be a hit of about $900M (1.2%) to the approximately $75B that hospitals receive under the OPPS (they get a lot more for inpatient care, but OPPS has been fast growing), but most hospitals will make about the same as last year because of the market basket update 

Conventional wisdom is that hospitals are too powerful and the administration will back off under pressure (expect wall to wall ads in DCA)
But I think this depends on
a) Will there be other groups (esp independent practices) supporting this change?
b) Does @SeemaCMS give a fig?
But I think this depends on
a) Will there be other groups (esp independent practices) supporting this change?
b) Does @SeemaCMS give a fig?
@SeemaCMS The truth is that this proposal could help hospitals be more competitive in value-based contracts/ alternative payment models, and they should embrace the changes.
If rural hospitals or AMCs need subsidies, then we should do it directly, not through distorting payment policies
If rural hospitals or AMCs need subsidies, then we should do it directly, not through distorting payment policies
• • •
Missing some Tweet in this thread? You can try to
force a refresh