NEW Analysis: Among people with employer coverage, nearly 1 in 5 inpatient admissions includes a claim from an out-of-network provider, putting them at risk for potentially high out-of-pocket costs. healthsystemtracker.org/brief/an-analy… @PetersonCHealth
Even when enrollees choose in-network facilities, a meaningful share of inpatient admissions result in the patient receiving a claim from an out-of-network provider. 

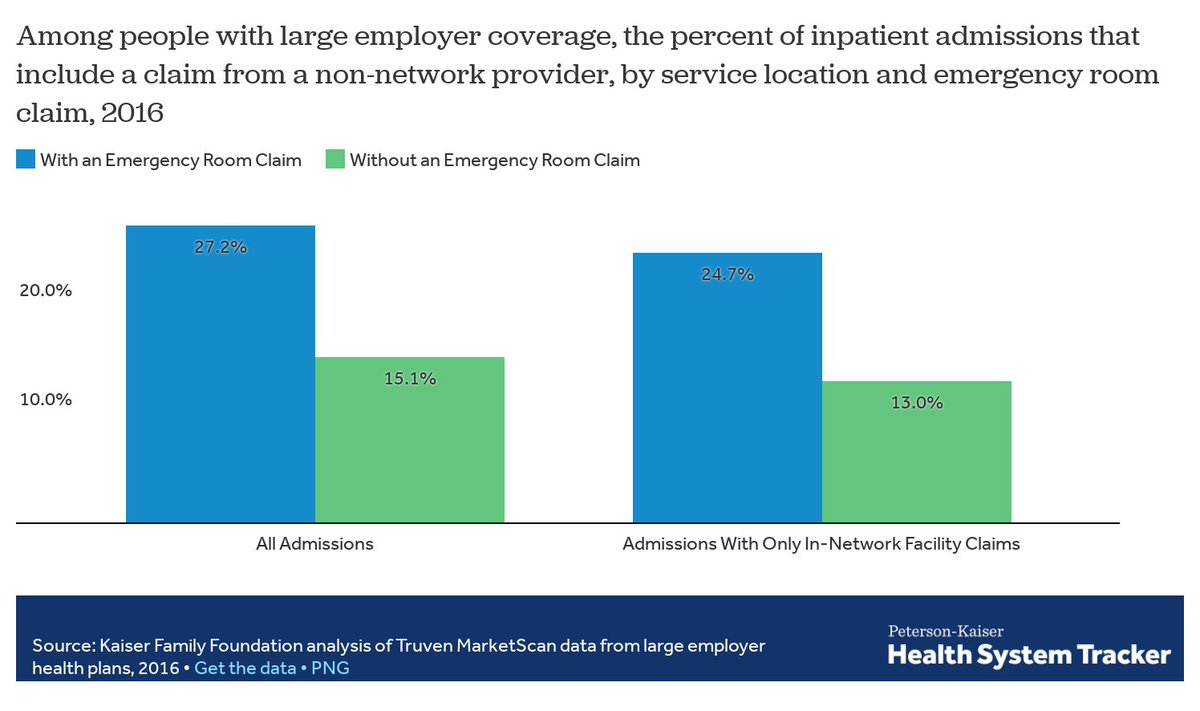
Emergency care is much more likely to include a claim from an out-of-network provider. This is true whether or not enrollees use in-network facilities. 
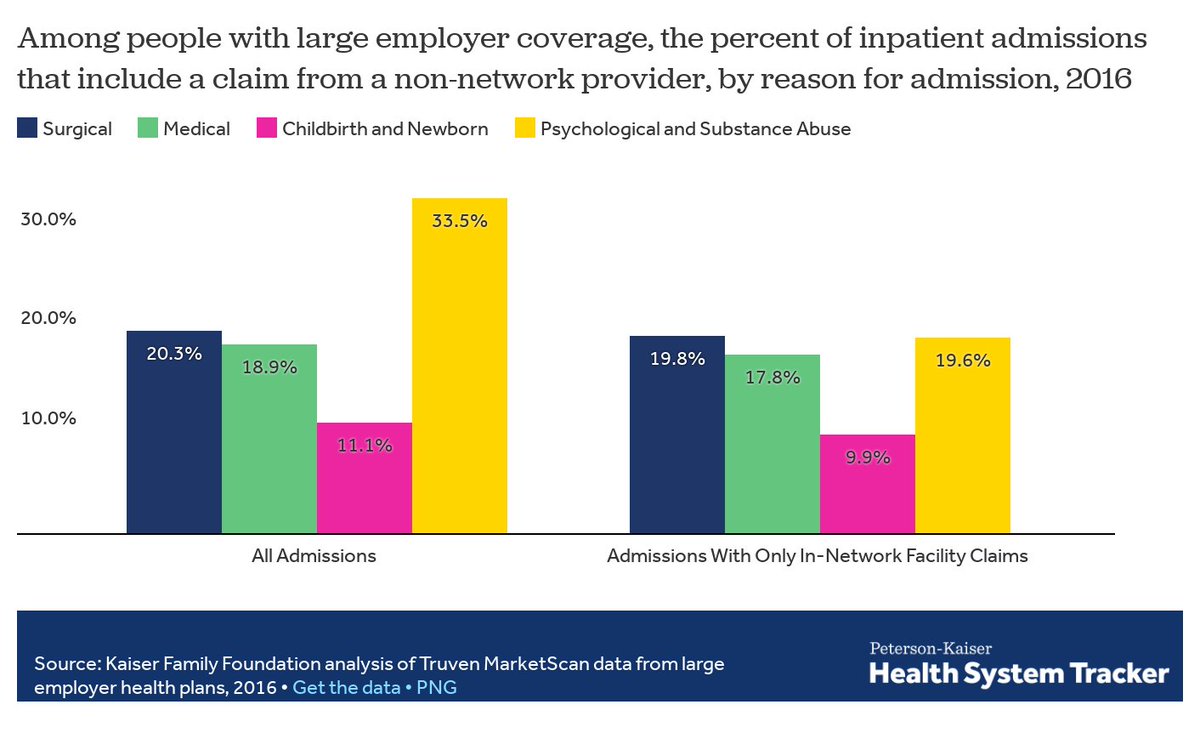
Admissions for #psychological or #SubstanceAbuse services also are much more likely to include an out-of-network provider claim, although enrollees who are able to receive care at an in-network facility significantly reduce their exposure. 
In some cases, patients may not be in a position to choose their provider -- for example, in emergencies or during surgery (e.g. anesthesiologists) -- and inadvertent out-of-network service use can result in a #SurpriseBill
Our analysis discusses some potential policy solutions for and hurdles to addressing surprise medical bills. For more on this, see @LorenAdler @BrookingsEcon healthaffairs.org/do/10.1377/hbl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh