1| follow for my critical appraisal tweetorial of #SCOTHEART trial in @NEJM #ESCCongress
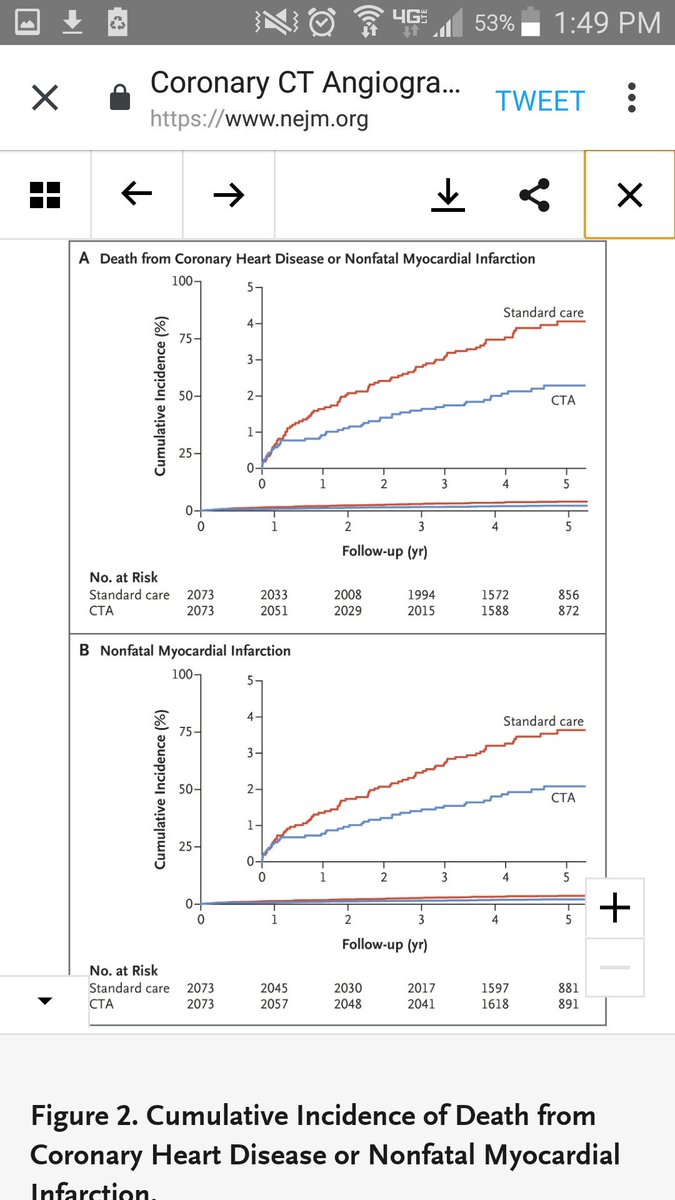
Basics: RCT of upfront CTA vs standard of care for stable CP referred to Scottish cardiology clinics. 1.6% fewer had primary outcome with CTA
nejm.org/doi/full/10.10…
Basics: RCT of upfront CTA vs standard of care for stable CP referred to Scottish cardiology clinics. 1.6% fewer had primary outcome with CTA
nejm.org/doi/full/10.10…
2| more basics: primary outcome is driven by nonfatal MI, not death. Authors did tremendous job at highlighting this
#ESCCongress #SCOTHEART
#ESCCongress #SCOTHEART
3| before diving in to methods/findings, how would a CTA first approach meaningfully change outcomes?
#ESCCongress
#ESCCongress
4| I would think CTA first strategy would work via both better revascularization and better medical therapies
5| hold onto that thought. 2 methods questions
Q: Was RCT blinded? A: no
Q: How were outcomes defined? A: dx codes, not adjudicated. See text below
#ESCCongress
Q: Was RCT blinded? A: no
Q: How were outcomes defined? A: dx codes, not adjudicated. See text below
#ESCCongress
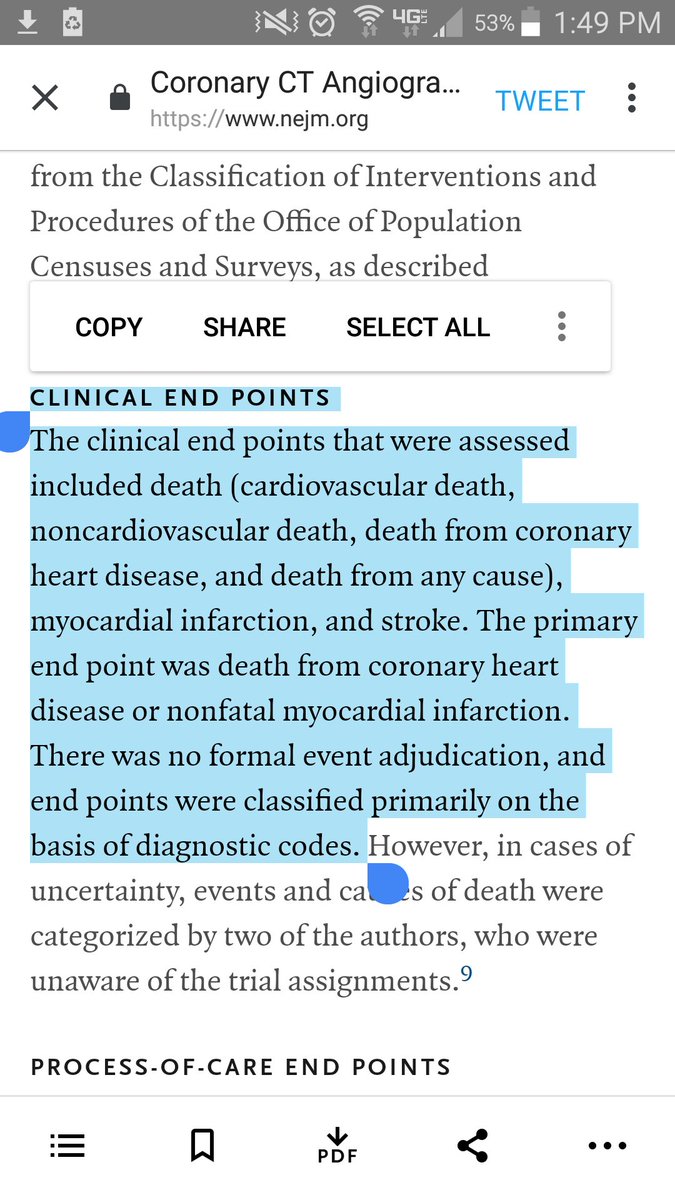
6| major limitation is having a bias susceptible primary outcome of non fatal MI. 1 reason is with CTA result in hand, could more easily classify MI as demand mismatch than true plaque rupture if had low CAC score
#ESCCongress
#ESCCongress
7| even if believe MI outcome safe from bias, did intermediate pathways on causal pathway improve?
For revascularization, NO
#ESCCongress
For revascularization, NO
#ESCCongress
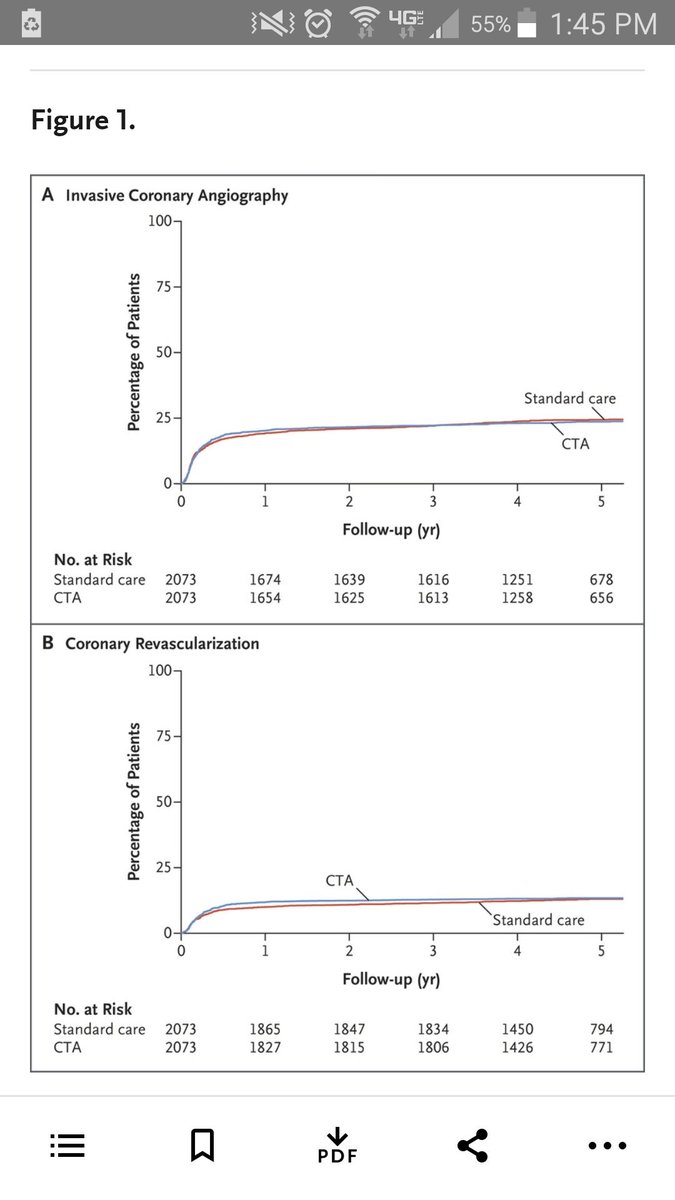
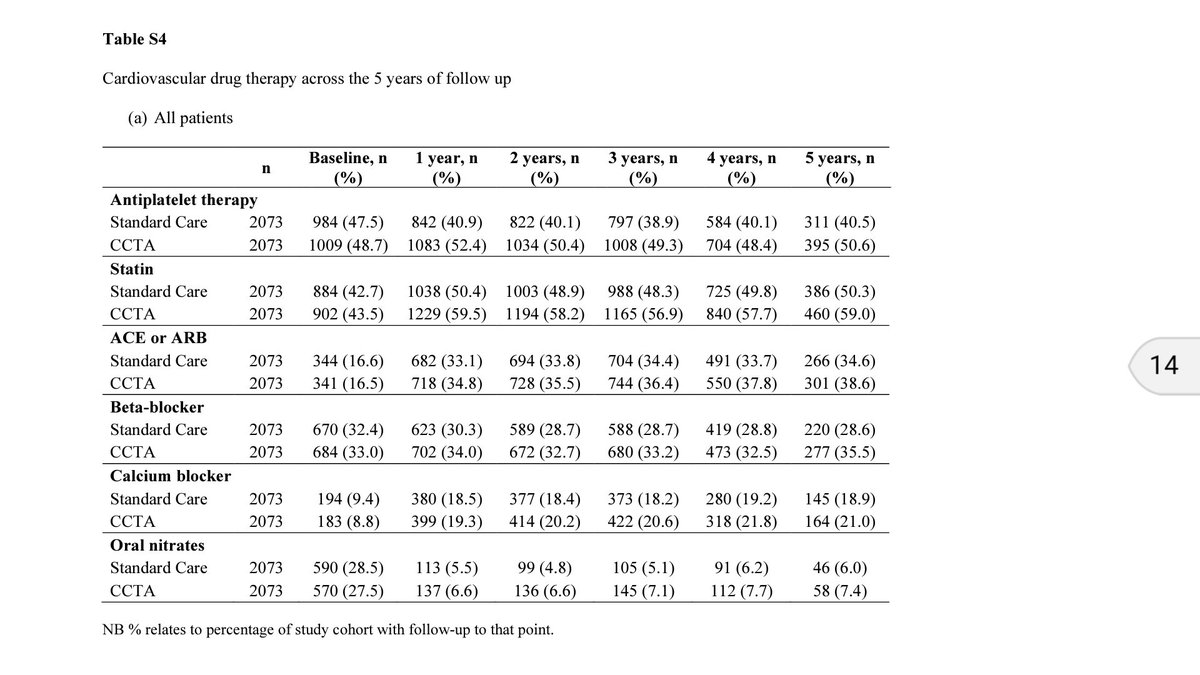
8| for optimal medical management, MODEST INCREASE in CTA group. 97 more people started treatment precisely.
#ESCCongress

#ESCCongress
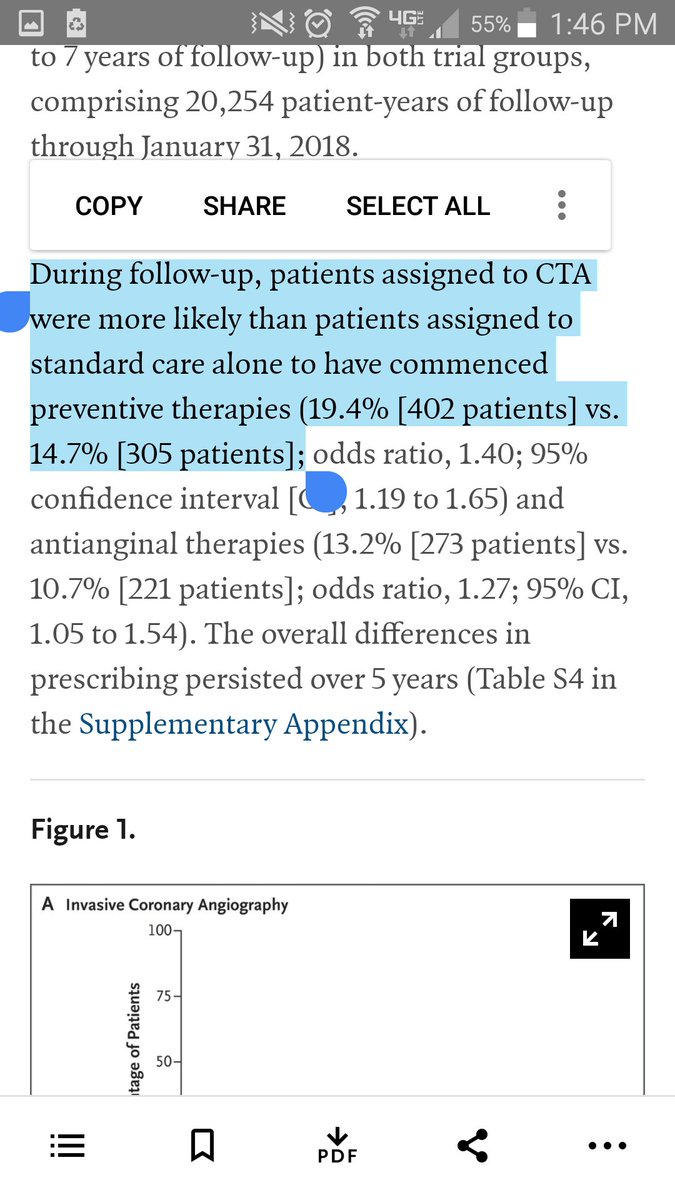
9| so with no real diff in PCI between groups, left to believe that 97 more ppl commencing therapy led to 29 fewer non fatal heart attacks. That would mean a NNT of 3 people after median follow up of 5 years!!!!
#ESCCongress
#ESCCongress
10| so to believe this result would mean having to believe medical therapy in a population with stable CP (many without CAD or angina) seen in an outpt carde clinic is far far more effective than ASA after STEMI (NNT in 40s)
11| my takeaway of #SCOTHEART trial: falls short due to: a)bias prone outcome of nonadjudicated nonfatal MI, b) CTA strategy without clear effect on necessary causal pathway for benefit, & c) implausible effect size of medical tx in low risk pop
#ESCCongress
Other takes?
#ESCCongress
Other takes?
12| 1 thing not reported is intensification of existing medical therapy. But dose dependent relationship only really strong for statins and not or nonexistent for BB, ACEi, or other antianginals.
#ESCCongress
End.
#ESCCongress
End.
• • •
Missing some Tweet in this thread? You can try to
force a refresh