1/ A little bit of history here…
When I was national coordinator for health IT, we did an RFI with CMS for “Advancing Interoperability and Health Information Exchange"
federalregister.gov/documents/2013…
When I was national coordinator for health IT, we did an RFI with CMS for “Advancing Interoperability and Health Information Exchange"
federalregister.gov/documents/2013…
https://twitter.com/Farzad_MD/status/988980496452419585
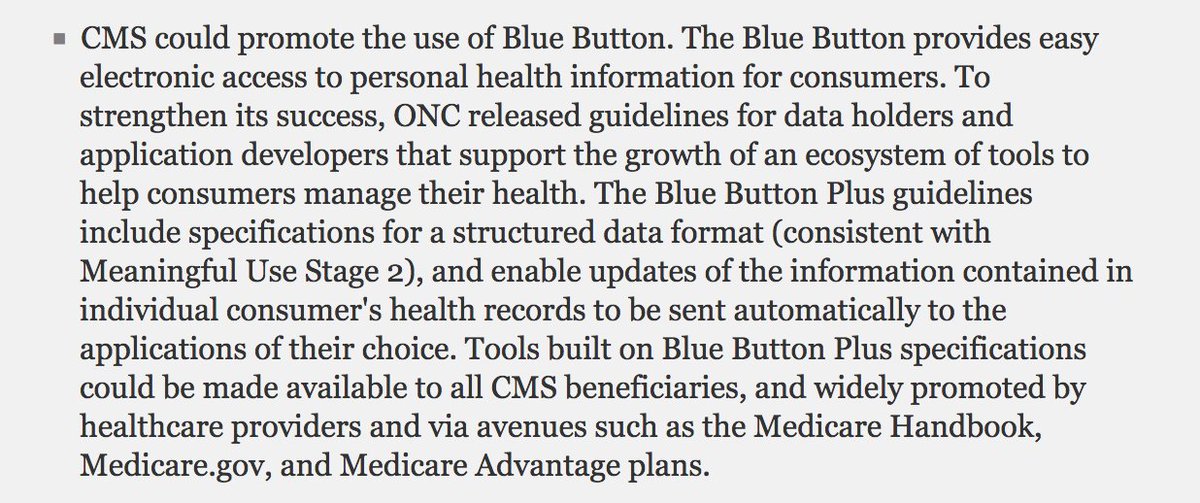
2/ If you’re a student of this stuff, it’s pretty topical- including a section on patient-centered information exchange on promoting #BlueButton - including through Medicare Advantage, … which is now on the verge of becoming a reality 
3/ Another idea I was pretty excited about was using inpatient/post-acute Conditions of Participation as a vehicle for getting information sharing - on the argument that it really is a basic health and safety requirement 

4/ We had a public session (with terrific colleagues Cindy Mann and @PatrickConwayMD) to discuss the RFI results, and sure enough, there was support for doing this
healthit.gov/sites/default/…

healthit.gov/sites/default/…
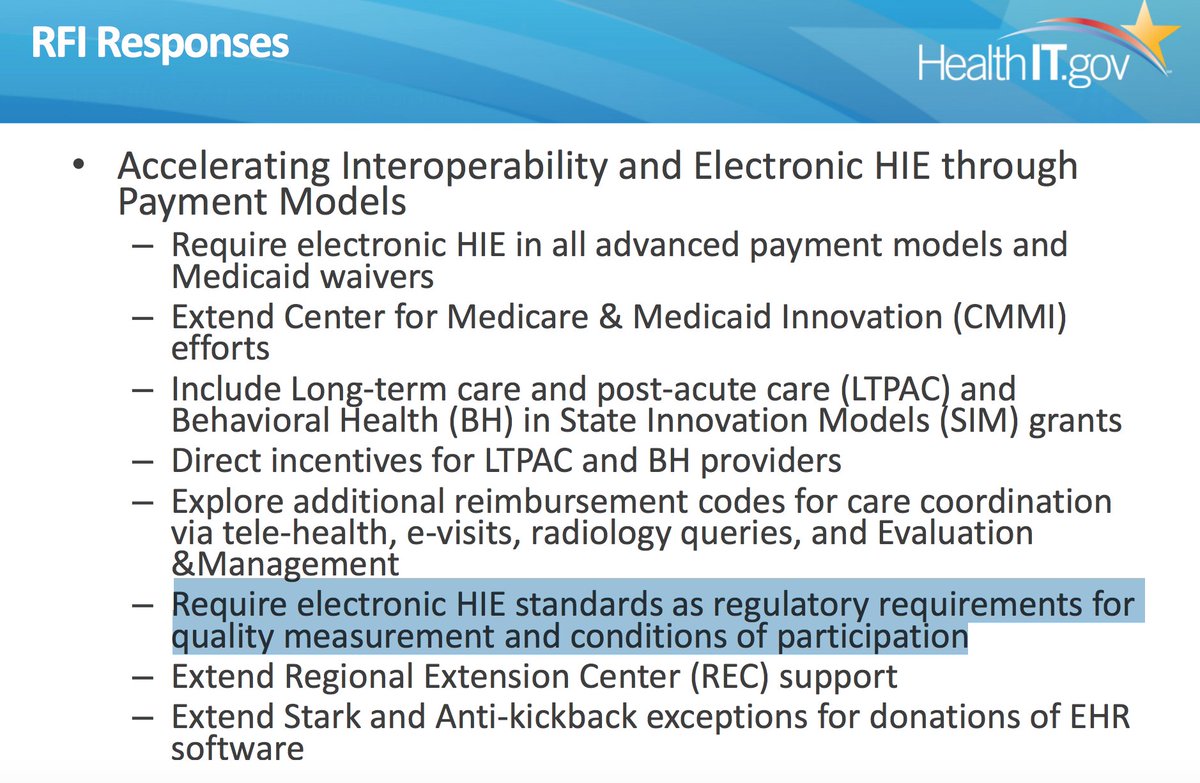

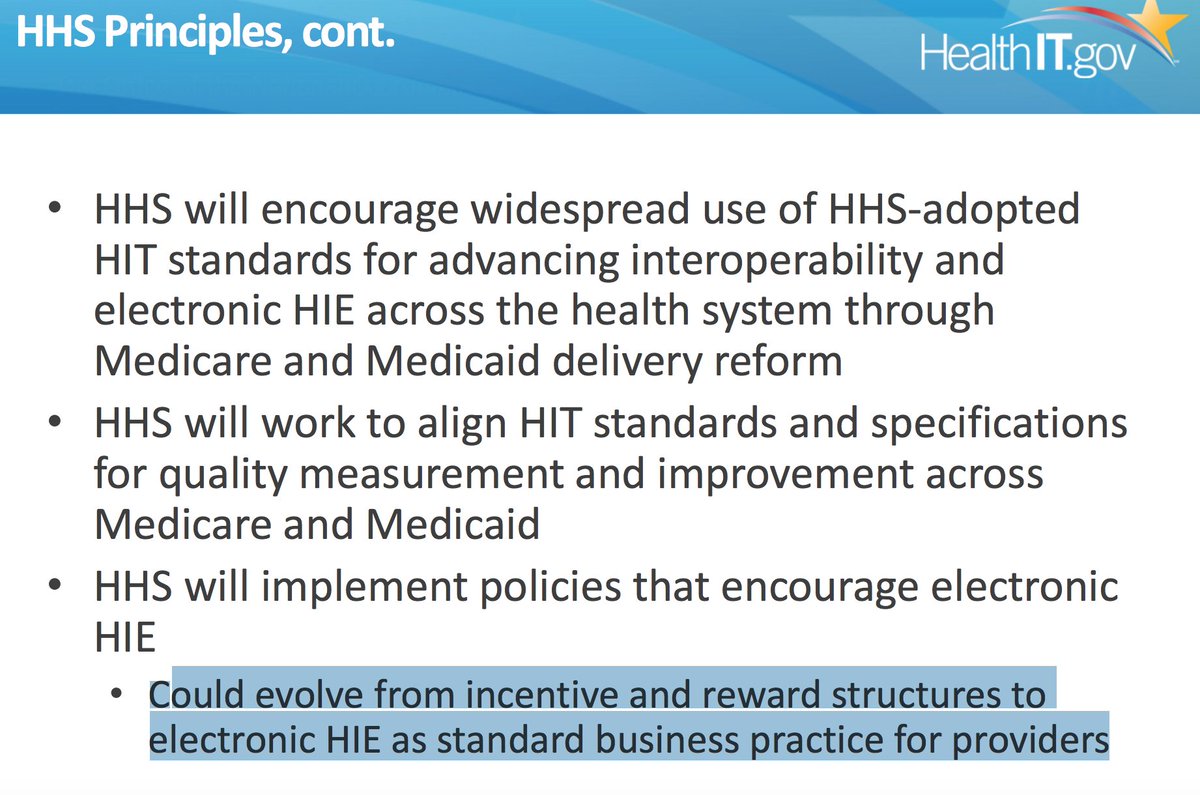
@PatrickConwayMD 5/ How this is framed was prescient:
HHS will implement policies that encourage electronic HIE
• Could evolve from incentive and reward structures to electronic HIE *as standard business practice* for providers
That’s what Condition of Participation means- it’s just expected
HHS will implement policies that encourage electronic HIE
• Could evolve from incentive and reward structures to electronic HIE *as standard business practice* for providers
That’s what Condition of Participation means- it’s just expected
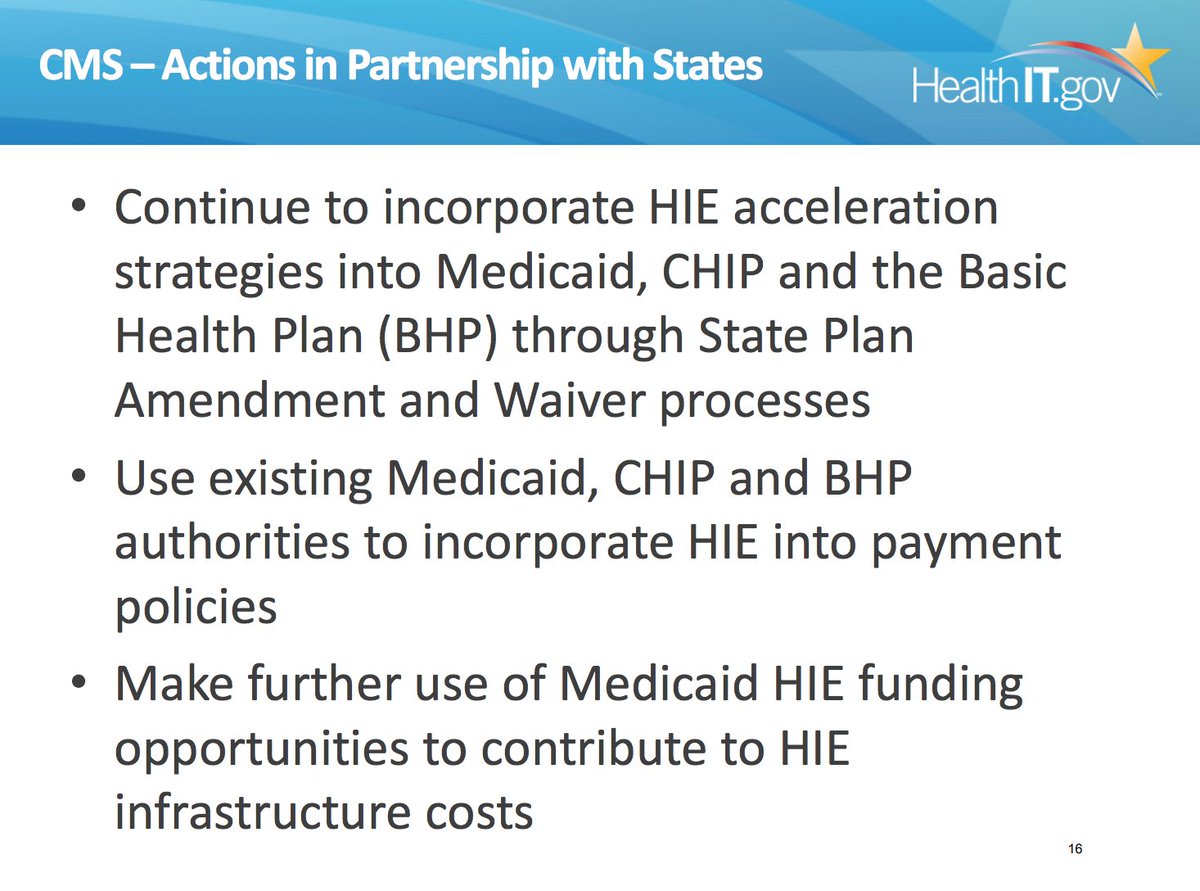
@PatrickConwayMD 6/ It also pointed to how Medicaid and State policies could encourage this data sharing-
HT/ @claudiawilliams @ThomasNOV @kdmertz @JessPKahn @julieboughn
• incorporate HIE into payment
policies
•Medicaid HIE funding
opportunities to contribute to HIE
infrastructure costs
HT/ @claudiawilliams @ThomasNOV @kdmertz @JessPKahn @julieboughn
• incorporate HIE into payment
policies
•Medicaid HIE funding
opportunities to contribute to HIE
infrastructure costs
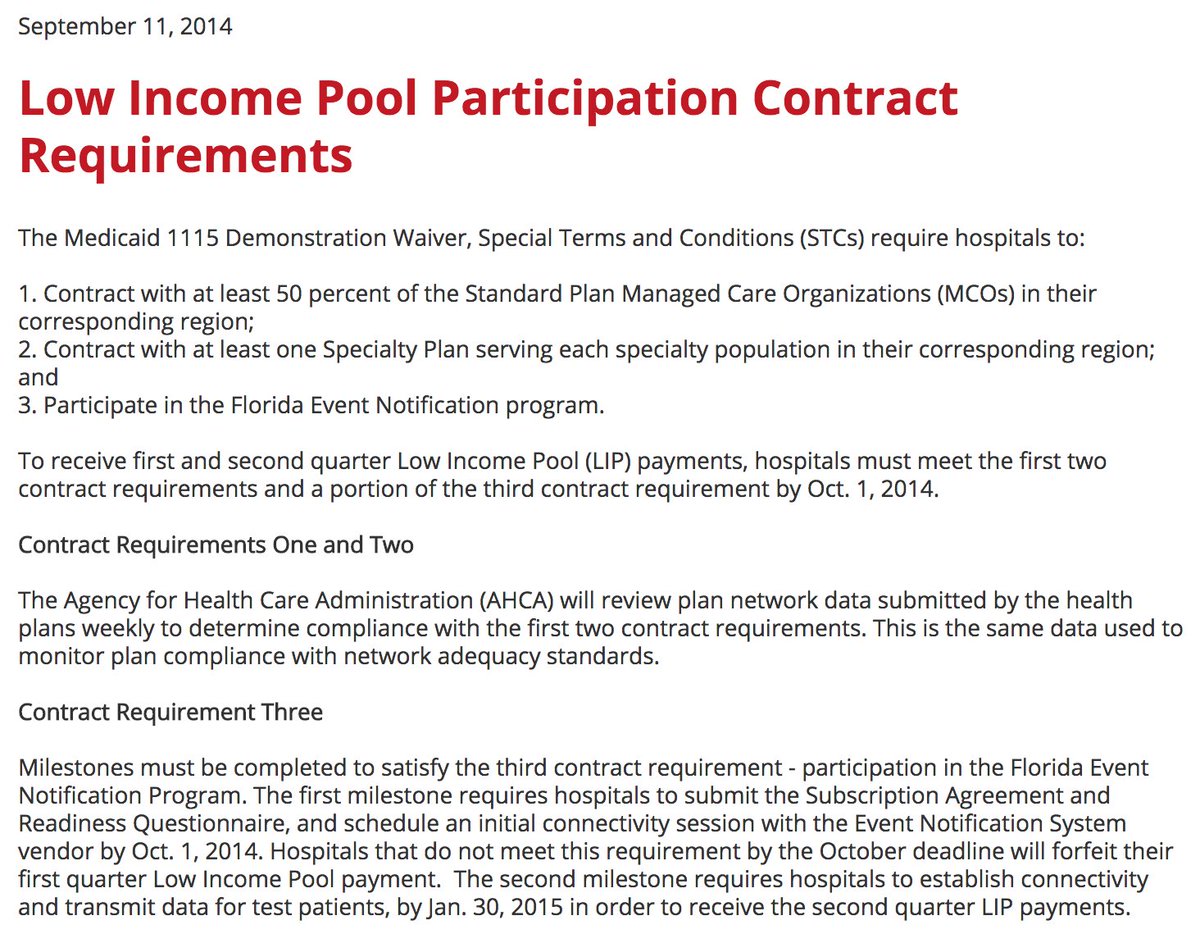
@PatrickConwayMD @claudiawilliams @ThomasNOV @kdmertz @JessPKahn @julieboughn 7/ Several states have taken up the mantle-
As part of their Medicaid #1115 demonstration waiver, Florida tied receipt of the low income pool payments to participation in the Florida Event Notification Program
participation went to almost 100% overnight
fha.org/advocacy/state…
As part of their Medicaid #1115 demonstration waiver, Florida tied receipt of the low income pool payments to participation in the Florida Event Notification Program
participation went to almost 100% overnight
fha.org/advocacy/state…
8/ What also bears mention is that THIS WAS NECESSARY TO GET UNIVERSAL HOSPITAL PARTICIPATION.
@AledadeACO is now operating in 20 states, and where discharge notifications are universally available are almost always where there is was a policy hook for hospital participation
@AledadeACO is now operating in 20 states, and where discharge notifications are universally available are almost always where there is was a policy hook for hospital participation
@AledadeACO 9/ This is what data blocking looks like- connecting to the health information exchange is
“a low priority”
“resource limited”
“waiting for EHR switchover to be completed”
and in unguarded moments..
“why would we give away data that’s a strategic asset?”
“join the hospital ACO"
“a low priority”
“resource limited”
“waiting for EHR switchover to be completed”
and in unguarded moments..
“why would we give away data that’s a strategic asset?”
“join the hospital ACO"
@AledadeACO 10/ So where are we 5 years later?
It is time.
As @SecAzar said, "it will require some degree of federal intervention — perhaps even an uncomfortable degree. That may sound surprising coming from an administration that deeply believes in the power of markets and competition."
It is time.
As @SecAzar said, "it will require some degree of federal intervention — perhaps even an uncomfortable degree. That may sound surprising coming from an administration that deeply believes in the power of markets and competition."
@AledadeACO @SecAzar 11/ The infrastructure is in place- we have spent billions on hospital EHR subsidies. Over 1B on state HIE infrastructure & governance
We have evidence from state demos that *it is possible* to share information if you are motivated
@SeemaCMS isn’t afraid of hospital lobby
We have evidence from state demos that *it is possible* to share information if you are motivated
@SeemaCMS isn’t afraid of hospital lobby
• • •
Missing some Tweet in this thread? You can try to
force a refresh