Evaluation of Cardiac Masses:
A Tweetorial for #FITSurvivalGuide 🚨 #ACCImaging @ASE360 @SCMR @journalofCMR @ACCinTouch
Dedicated:@dr_chirumamilla & all #ACCFIT in #CardioTwitter
Main Ref: link.springer.com/article/10.100… Palaskas, et al. Curr Treat Options Cardio Med (2018) 20: 29.
A Tweetorial for #FITSurvivalGuide 🚨 #ACCImaging @ASE360 @SCMR @journalofCMR @ACCinTouch
Dedicated:@dr_chirumamilla & all #ACCFIT in #CardioTwitter
Main Ref: link.springer.com/article/10.100… Palaskas, et al. Curr Treat Options Cardio Med (2018) 20: 29.

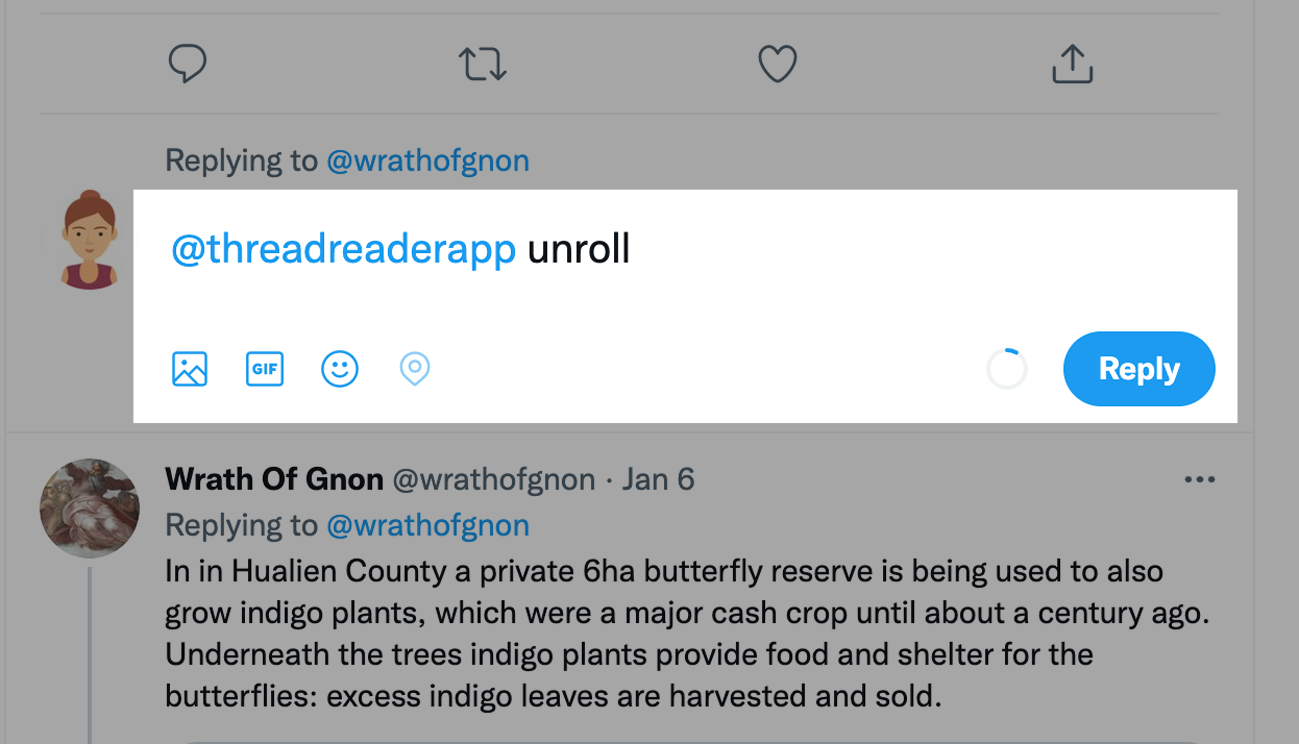
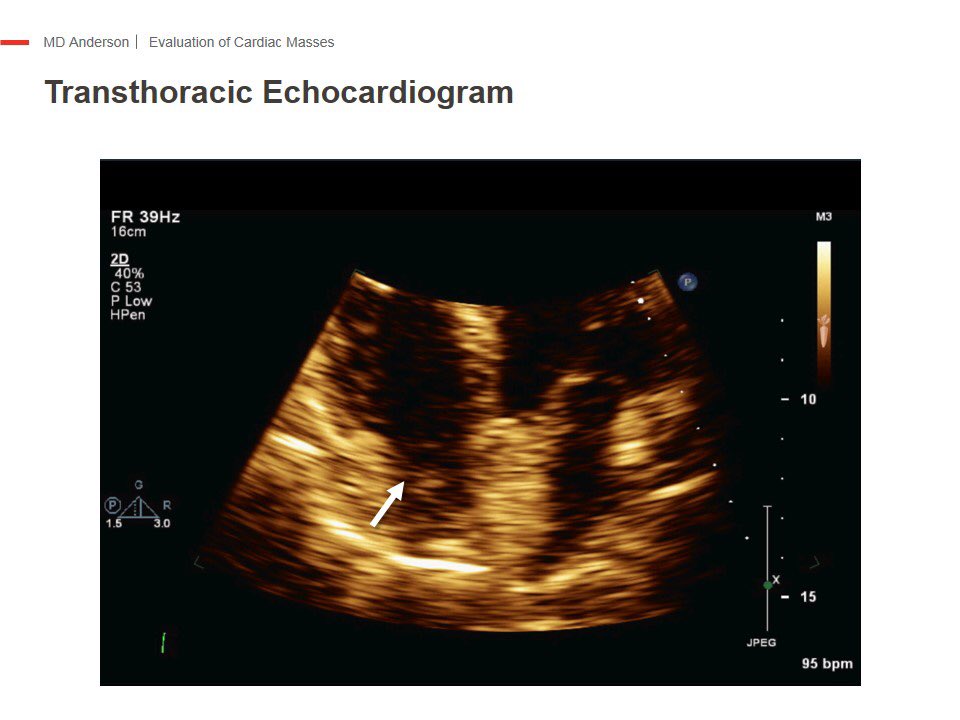
Usually, it all starts with an abnormal finding in an echo suggestive of intracavitary mass. How can we tell one from the other? It can be confusing. 

For artifacts, I did a Tweetorial already that describes the most common ones. Basic understanding of ultrasound physics is needed to be able to explain them: twitter.com/i/moments/1030…
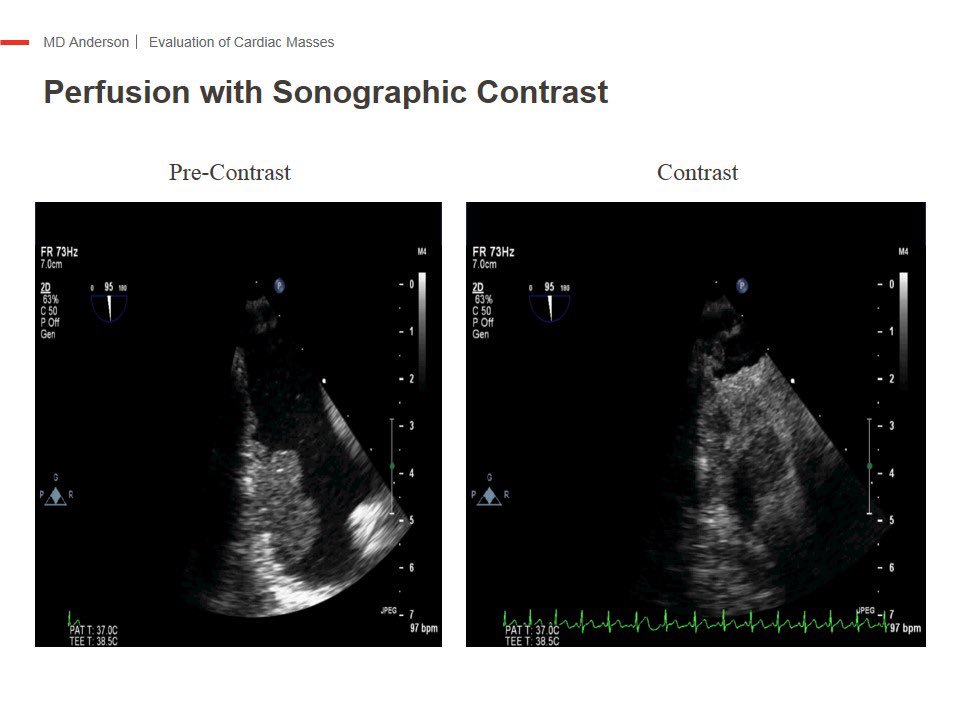
TTE with U/S enhancing agent (UEA) can be very helpful in cases that are borderline/suspicious or not able to tell artifact vs. real mass, if regular 2D TTE using color Doppler, optimizing time-gain compensation, lowering gain and acquiring other imaging planes are not helpful.
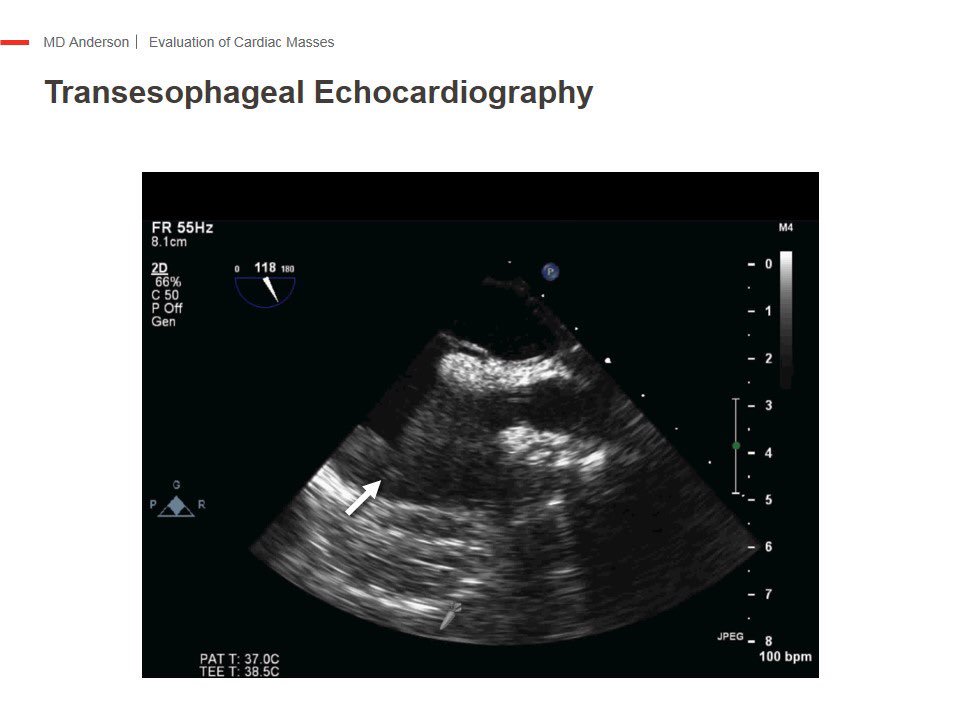
Same case with color Doppler, showing suspiciously evidence of vascularization. Small vessels within the RV apical mass show flow as small speckles
In case you weren’t convinced, look at evidence of perfusion with injection of UEA aka “contrast”. The mass has perfusion. Thrombus will be of course avascular.
The use of UEA in a case with suspected mass is a must. Even if the mass or thickened part of the heart is not suspected to be a thrombus. Always helpful.
So in summary, so far we can say:
🌕Tumor Characteristics in #EchoFirst:
1️⃣No associated segmental wall motion abnormalities following CAD territory.
2️⃣Typically normal LVEF
3️⃣Invasive appearance
4️⃣Atypical location
5️⃣ Perfusion with UEA.
🌕Tumor Characteristics in #EchoFirst:
1️⃣No associated segmental wall motion abnormalities following CAD territory.
2️⃣Typically normal LVEF
3️⃣Invasive appearance
4️⃣Atypical location
5️⃣ Perfusion with UEA.
Very important to place location & clinical context into all of this. We don’t need to do multimodality imaging in all thrombi. For example, a pt with A-fib & a free floating mass or a mass in LAA, doesn’t need a CMR, just anticoagulantion. Same w/pt with Hx LAD MI & mass at apex
Typical appearance of a papillary fibroelastoma. Coliflower. I hope @purviparwani doesn’t get triggered by this.🤭 Be familiar with this one, usually location is in the aortic side of aortic valve. Risk of embolism is high. The good news is that is benign.
Another primary benign cardiac tumor is myxoma. Usually attached to the interatrial septum by a stalk & typically in left atrium. If large enough can cause obstructive symptoms. Constitutional symptoms too.Treatment is surgical. Can recurr. Read a little bit about Carney Complex.
Also, don’t forget to look at the pericardium. Is not always epicardial fat. In this case, 2D TTE w/ color Doppler was very helpful in identifying vascularization in a pericardial tumor.
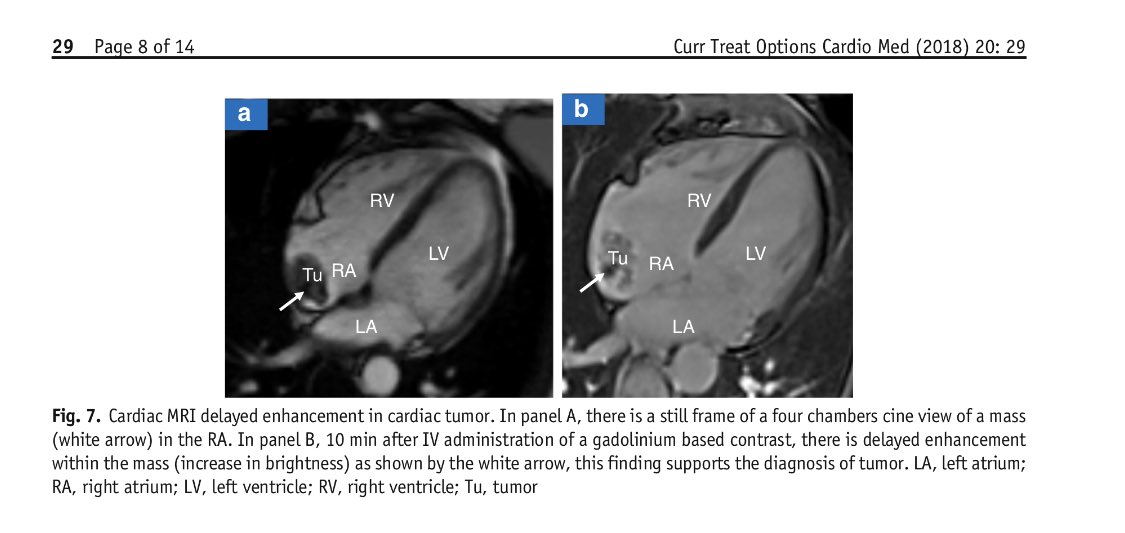
Primary malignant cardiac tumors, like sarcoma are rare, but very difficult to treat. They tend to recur even when resection has -ve margins. These pts should be treated in or comanaged in specialized cancer centers. An example below. Look at all that gadolinium enhancement. 
Cardiac metastatic disease is far more common than sarcomas, important to understand that when cardiac mets are identified in a patient, survival is similar to Stage IV cancers. Execept, renal cell CA IVC tumor-thrombus extensión to RA, these pts do very well with surgery & chemo
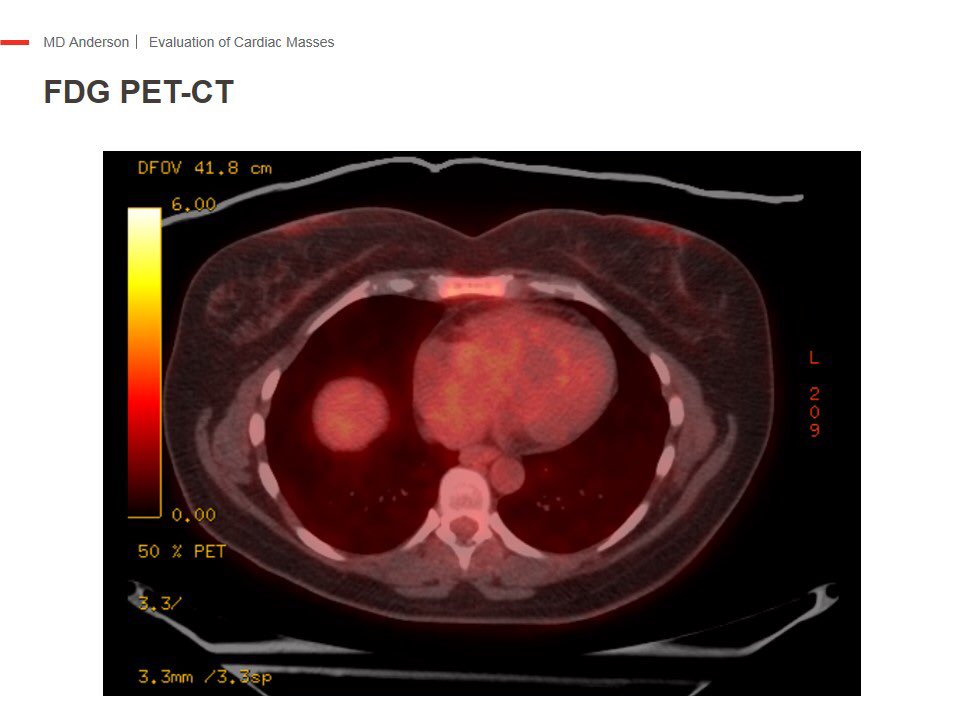
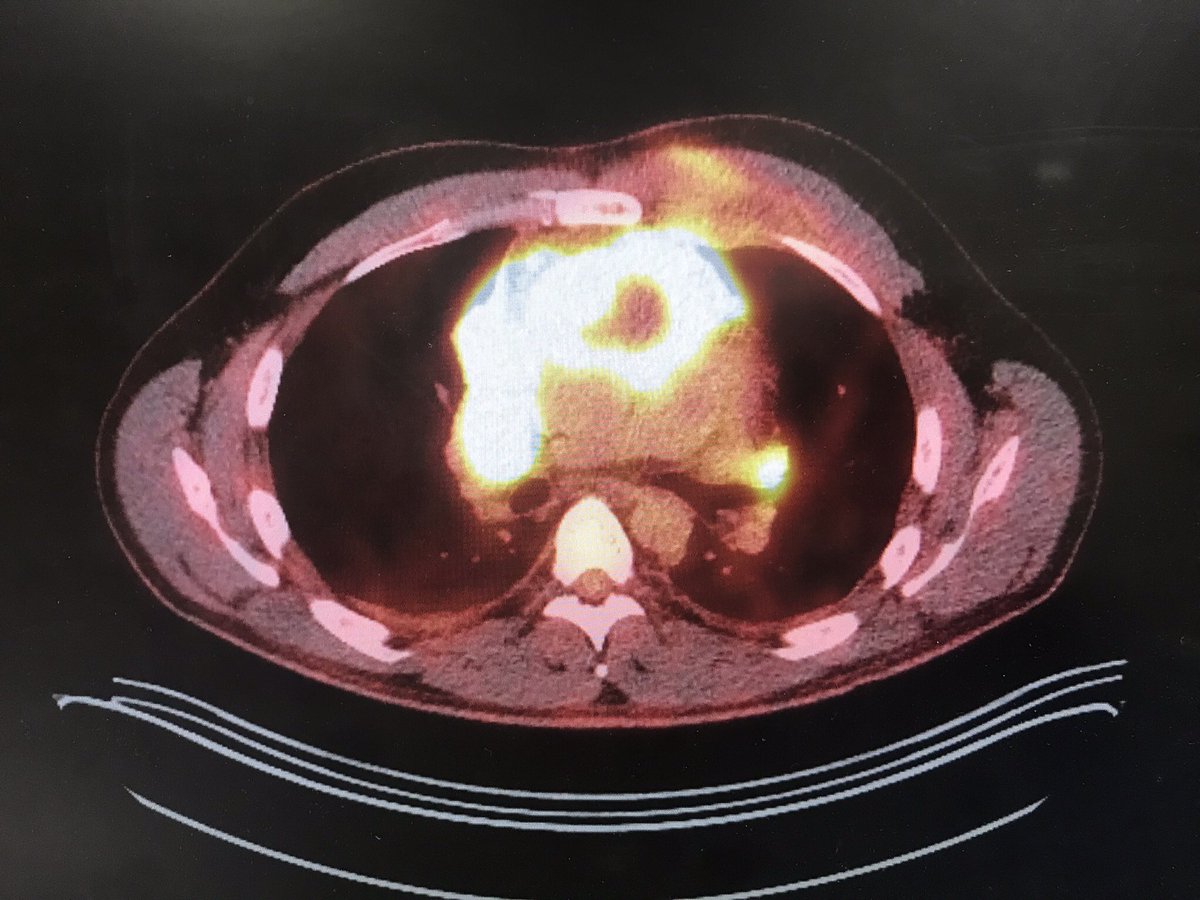
Because cardiac mets are more common than 1ry malignant tumors, we recommend to do a PET-CT in all pts when Dx by CV imaging is tumor, before starting to think about surgical resection or open bx. Very helpful if there is an advanced undiagnosed malignancy. 
#WhyCMR should be performed in all cardiac tumors, because it adds more anatomical info for surgical purposes, or if percutaneous bx is decided. Check our approach in this proof of concept case series: imaging.onlinejacc.org/content/11/8/1…
For thrombus, the best non-invasive technique to differentiate them from tumor is #whyCMR. Excellent work by Jon Weinsaft, showing how the presence of thrombus in CMR using long inversion time LGE Imaging was related to clinical events & histology when thrombus was identified. 
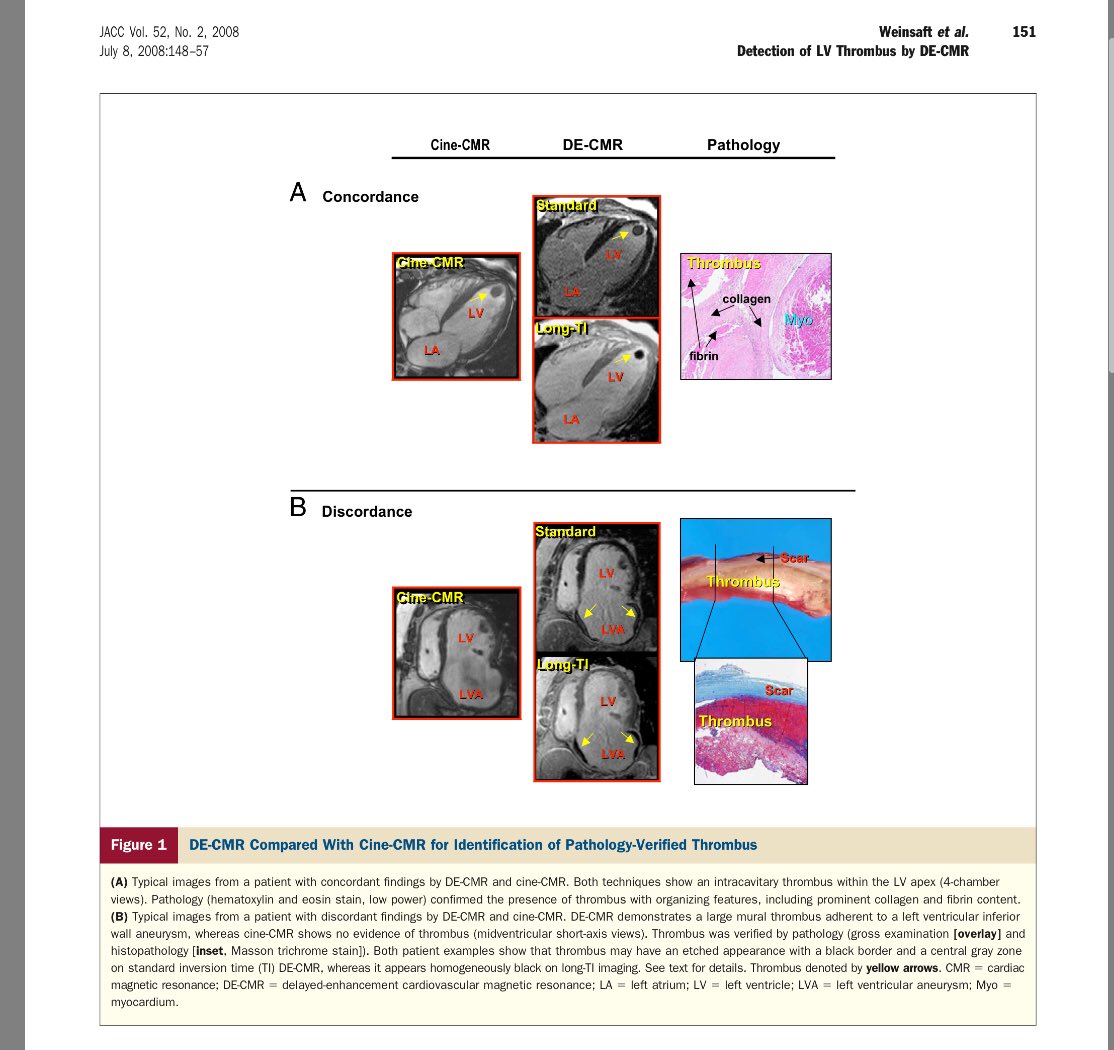
One of many examples. Thrombus associated with old anterior MI. CMR was done to assess viability. See how the thrombus is jet black? 

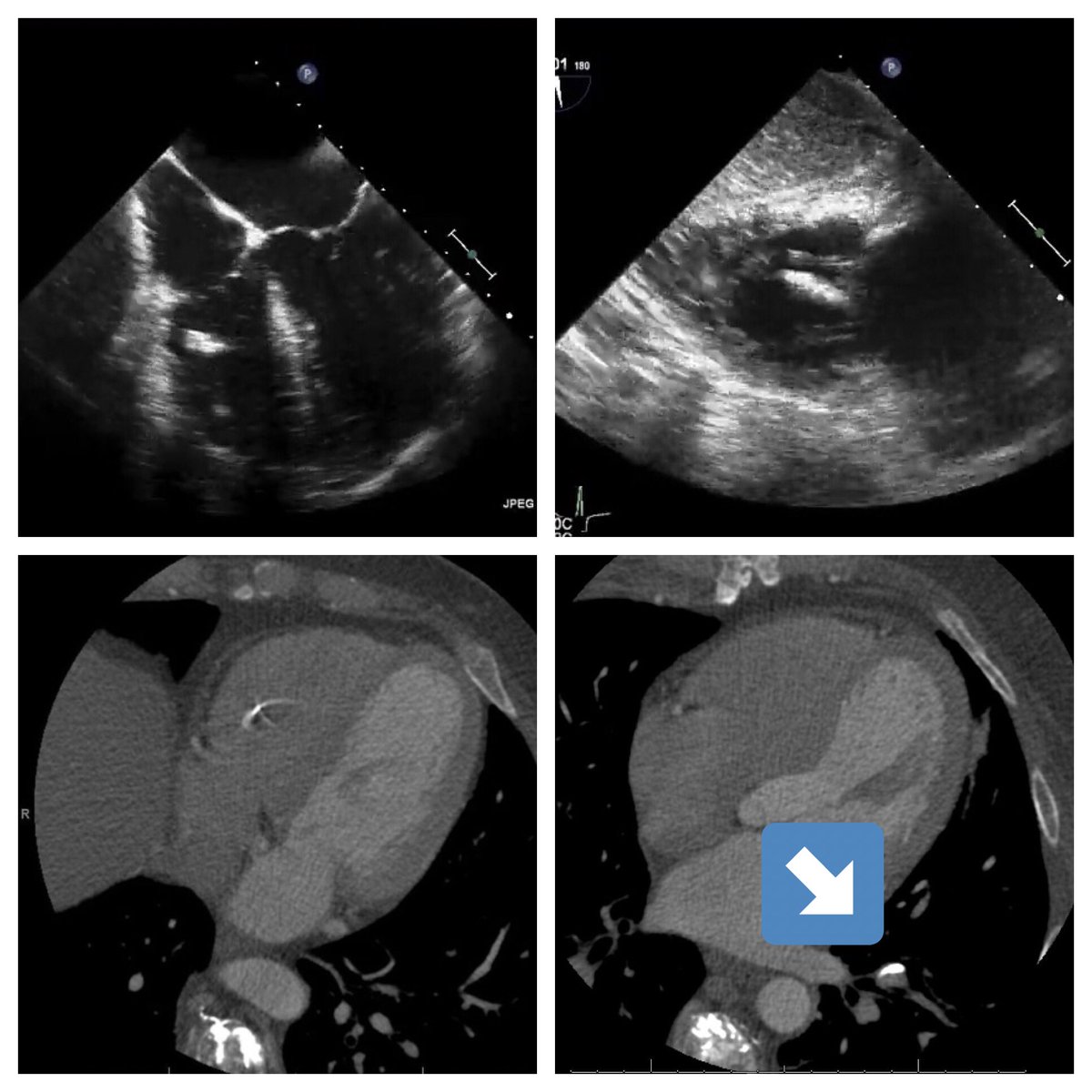
CT Houndsfield units overlap, so not a good option to identify thrombus. Less specificity. Sorry @AChoiHeart . 😂
In selected cases I’ve used CT. Especially if mass highly calcified, which in CMR, they will look like thrombus. Lady with myeloma, that I did the TEE & still was unhappy. With #YesSCCT we could identify that spine injection of bone cement embolized to heart & lung circulation. 
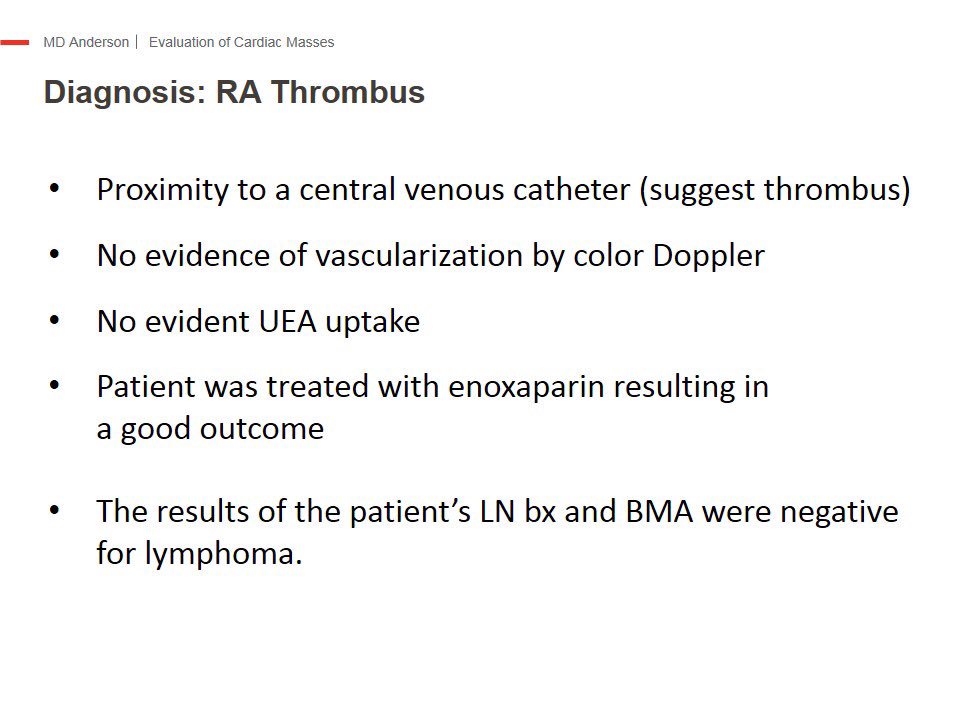
Putting it all together. Thrombus echo characteristics are generally the opposite of tumor. For UEA, absence of perfusion not necessarily means thrombus. Below you can see our algorithm. 

This is a compendium of the most important concepts for evaluation of cardiac masses. Unfortunately there are no guidelines or formal standardization of this knowledge. I believe & have tried to engage imaging societies to develop an endorsed approach. More to come, hopefully.
*Cauliflower
• • •
Missing some Tweet in this thread? You can try to
force a refresh