Discover and read the best of Twitter Threads about #FiTSurvivalGuide
Most recents (24)
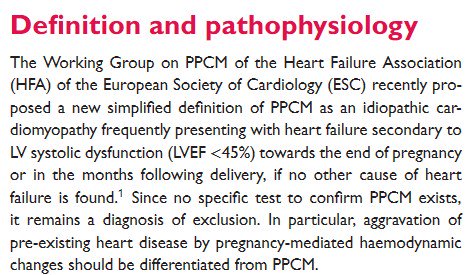
#FITSurvivalGuide: CV disease in Pregnancy #CardioObstetrics
#Tweetorial for new #CardiologyFIT by @MonSangh and @JennLewey @Penn
1⃣CV Physiology
2⃣Peripartum CM
3⃣SCAD
4⃣Valve Dz
5⃣Aortopathy
6⃣Arrhythmias
7⃣HTN Disorders of 🤰
8⃣🤰& Future CV Risk
9⃣Drug Safety
#Tweetorial for new #CardiologyFIT by @MonSangh and @JennLewey @Penn
1⃣CV Physiology
2⃣Peripartum CM
3⃣SCAD
4⃣Valve Dz
5⃣Aortopathy
6⃣Arrhythmias
7⃣HTN Disorders of 🤰
8⃣🤰& Future CV Risk
9⃣Drug Safety
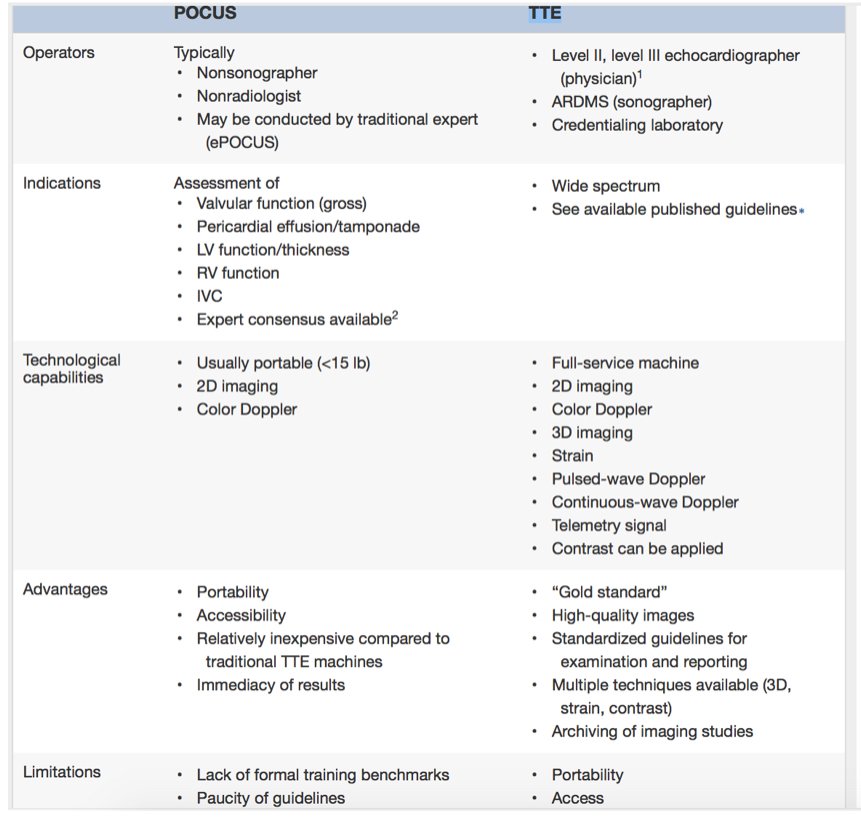
Curious about how #POCUS is taught? This #Tweetorial is for U
#Preview for #ASEchoJC 🔜9/4 8pm EST
Point-of-Care Cardiac Ultrasound POCUS: State-of-the-Art in Medical School Education bit.ly/2wxD4PZ by @amerjohri
#POCUS not 🐇🎩, not short #TTE



#Preview for #ASEchoJC 🔜9/4 8pm EST
Point-of-Care Cardiac Ultrasound POCUS: State-of-the-Art in Medical School Education bit.ly/2wxD4PZ by @amerjohri
#POCUS not 🐇🎩, not short #TTE
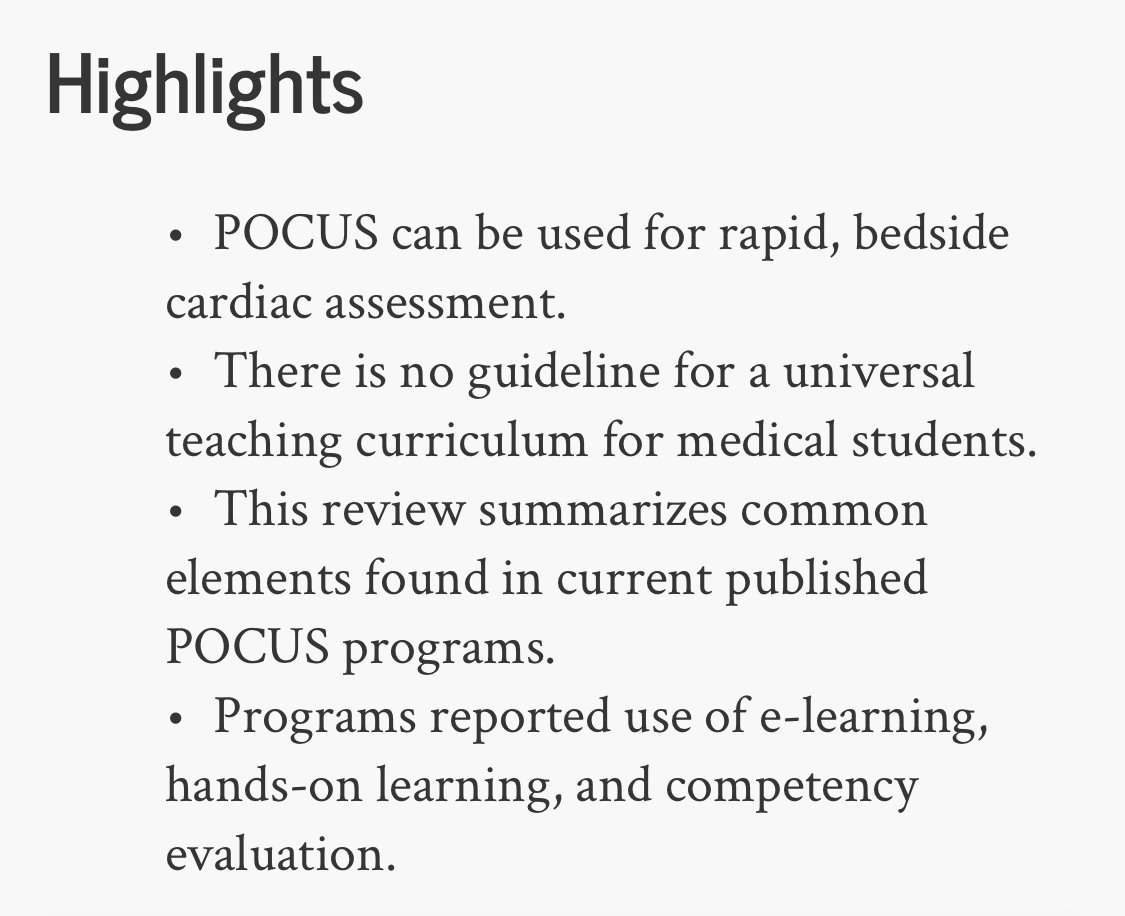

2/ Current #goals #Cardiac #POCUS #MedEd
(1) introduce concepts of ultrasound- common imaging views, correlate with anatomy, & physical examination skills
(2) develop scanning techniques➡️ basic competence
(3) recognize & differentiate b/w normal anatomy & basic pathology



(1) introduce concepts of ultrasound- common imaging views, correlate with anatomy, & physical examination skills
(2) develop scanning techniques➡️ basic competence
(3) recognize & differentiate b/w normal anatomy & basic pathology


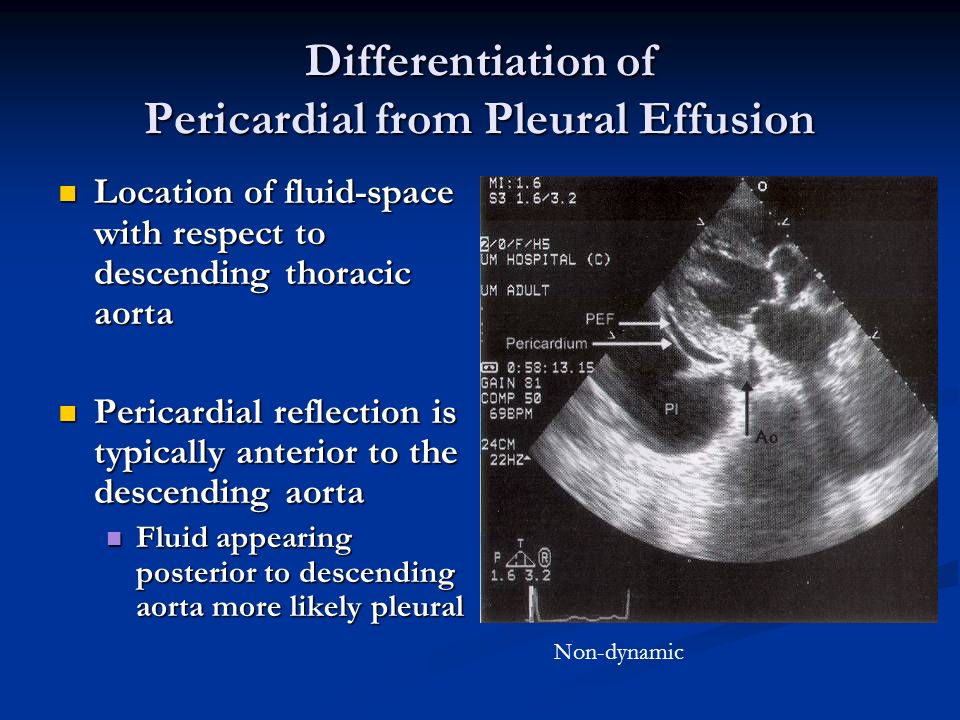
3/ When Do We Start? Prerequisite knowledge for #POCUS teaching
"priming effect" of preclinical education
Big machine 1st over handheld Martinez et al bit.ly/2wzCcJB @UMMC
Start 1st year @Hoppmann et al bit.ly/2Q4ECsO @UofSCSOM
"priming effect" of preclinical education
Big machine 1st over handheld Martinez et al bit.ly/2wzCcJB @UMMC
Start 1st year @Hoppmann et al bit.ly/2Q4ECsO @UofSCSOM
Another #FITSurvivalGuide tweetorial. This time on #intracoronary imaging w/ focus on IVUS and OCT
➡️ Rationale for use
➡️ Tech basics
➡️ Uses
➡️ Data
➡️ Images (high-yield)
➡️Comparison
@z_alirhayim @Almanfi_Cardio @AntoniousAttall @abashirMD @Babar_Basir

➡️ Rationale for use
➡️ Tech basics
➡️ Uses
➡️ Data
➡️ Images (high-yield)
➡️Comparison
@z_alirhayim @Almanfi_Cardio @AntoniousAttall @abashirMD @Babar_Basir
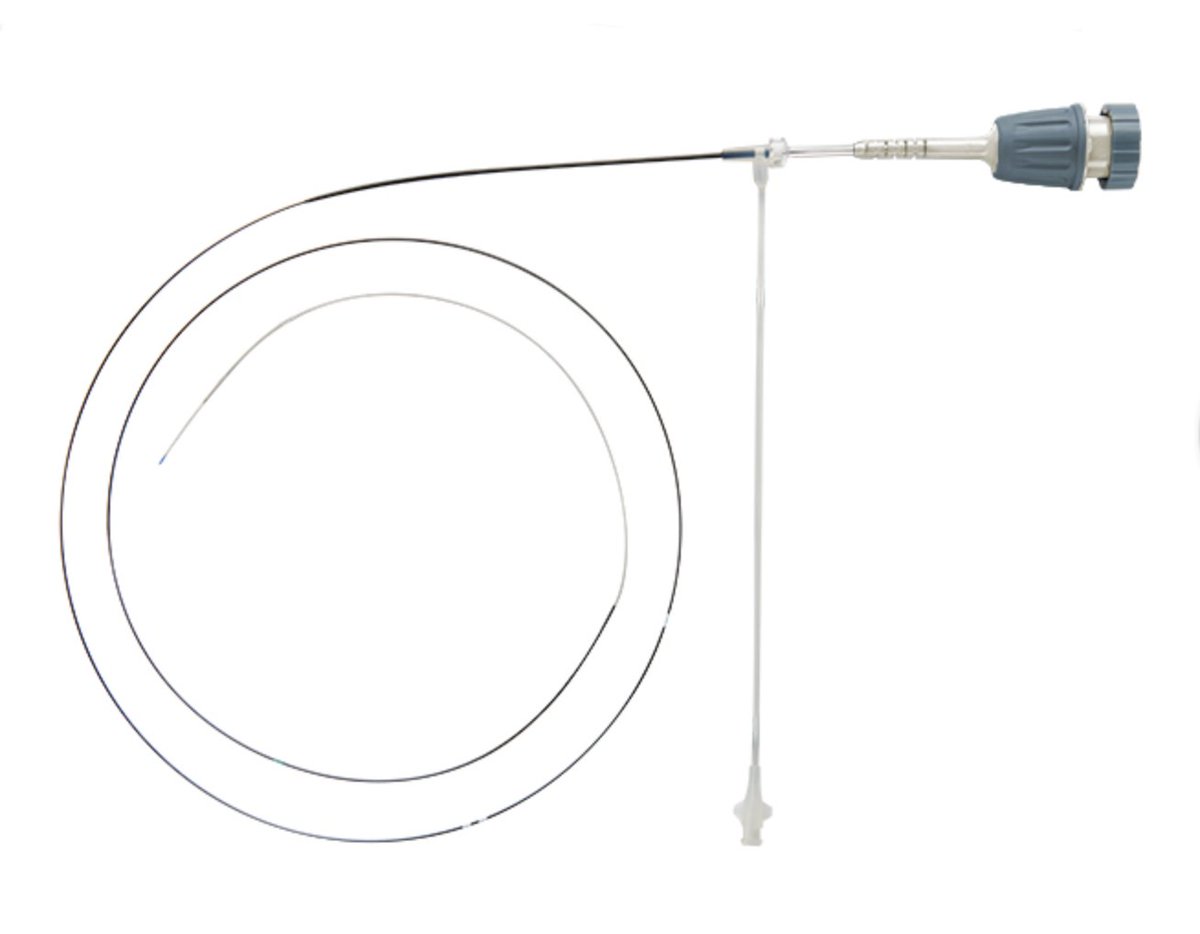

Why use them?
- Cor angio limited by: 2D view of 3D artery, diffuse dx, foreshortening, angulations, Ca++, eccentricity, vessel overlap, contrast streaming
- Angio alone ➡️ undetected edge complications, suboptimal stent exp in 15-20% ➡️ adverse events @cardiojaydoc02
- Cor angio limited by: 2D view of 3D artery, diffuse dx, foreshortening, angulations, Ca++, eccentricity, vessel overlap, contrast streaming
- Angio alone ➡️ undetected edge complications, suboptimal stent exp in 15-20% ➡️ adverse events @cardiojaydoc02
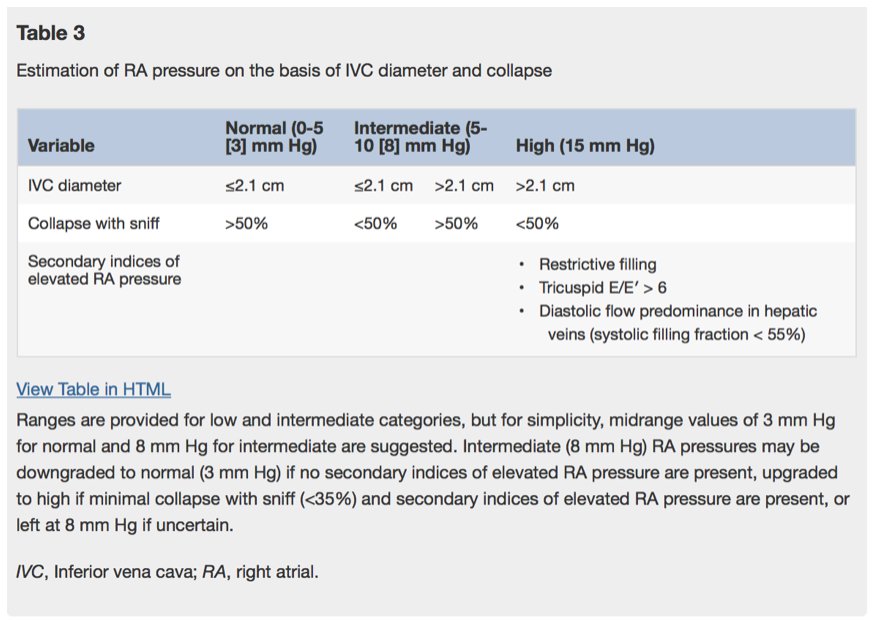
#FITSurvivalGuide - Right Heart Catheterizations
1⃣&2⃣ - Applications
3⃣ , 4⃣ , 5⃣ & 6⃣ - Data: Pressures, PCWP Waveform, CO & Shunts
7⃣ - Complications
Take home: RHC = useful diagnostic tool. Safe & effective use depends on thoughtful placement and data intepretation
1⃣&2⃣ - Applications
3⃣ , 4⃣ , 5⃣ & 6⃣ - Data: Pressures, PCWP Waveform, CO & Shunts
7⃣ - Complications
Take home: RHC = useful diagnostic tool. Safe & effective use depends on thoughtful placement and data intepretation
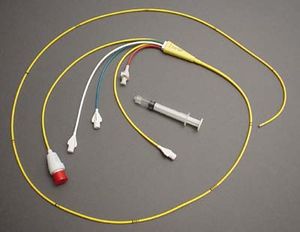
#FITSurvivalGuide - Right Heart Catheterizations
1⃣ - Applications
Accurate assessment of hemodynamics and etiology of shock
Assessment and management of severe HF e.g. "tailored therapy"
Evaluations of intracardiac shunts, valvular lesions
Perioperative management of severe HF
1⃣ - Applications
Accurate assessment of hemodynamics and etiology of shock
Assessment and management of severe HF e.g. "tailored therapy"
Evaluations of intracardiac shunts, valvular lesions
Perioperative management of severe HF
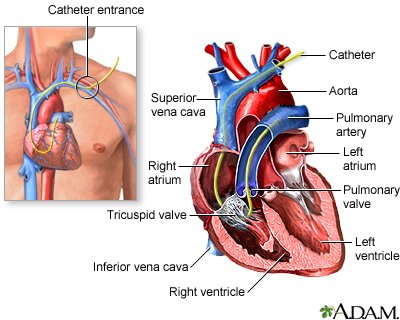
#FITSurvivalGuide - Right Heart Catheterizations
2⃣ - Applications
Risk stratification for patients considered for ❤️ Xplant
Establishing dx of PAH vs. secondary PH
Ddx: ❤️ vs non-❤️ cause of pulm edema (*caveat: RHC not indicated for routine mgmt of pulm edema or CHF)
2⃣ - Applications
Risk stratification for patients considered for ❤️ Xplant
Establishing dx of PAH vs. secondary PH
Ddx: ❤️ vs non-❤️ cause of pulm edema (*caveat: RHC not indicated for routine mgmt of pulm edema or CHF)

1/
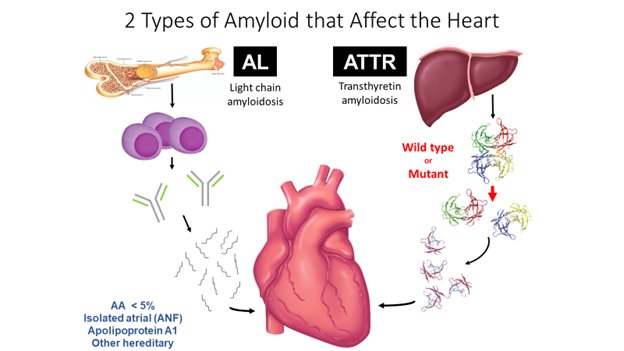
As #ESCCongress nears, I thought I would do a #tweetorial on amyloidosis. Exciting times for the field and new data/treatments expected next week.
#FITSurvivalGuide #CardioTwitter @tony_breu @rodney_falk @marthagrogan1 @amyloidosisfdn @AmyloidosisSupp @Amyloidosis_ARC
As #ESCCongress nears, I thought I would do a #tweetorial on amyloidosis. Exciting times for the field and new data/treatments expected next week.
#FITSurvivalGuide #CardioTwitter @tony_breu @rodney_falk @marthagrogan1 @amyloidosisfdn @AmyloidosisSupp @Amyloidosis_ARC
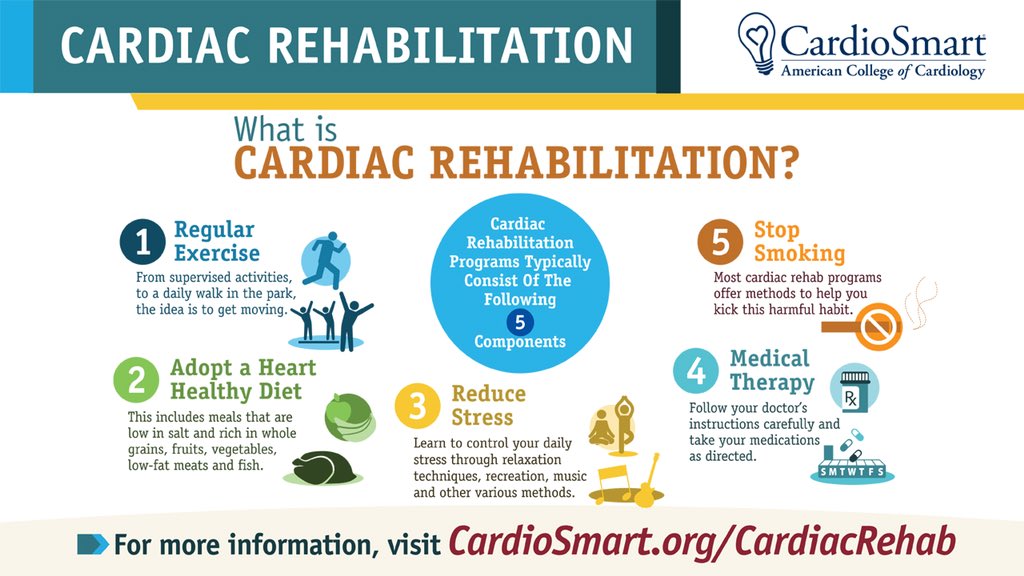
1/10 Cardiac Rehab – Secondary prevention #FITSurvivalGuide
1⃣Key Components
2⃣Benefits
3⃣Patients
4⃣Starting
5⃣Objective data
6⃣Patient limitations
7⃣Phase 1
8⃣Phase 2
9⃣Phase 3
1⃣Key Components
2⃣Benefits
3⃣Patients
4⃣Starting
5⃣Objective data
6⃣Patient limitations
7⃣Phase 1
8⃣Phase 2
9⃣Phase 3
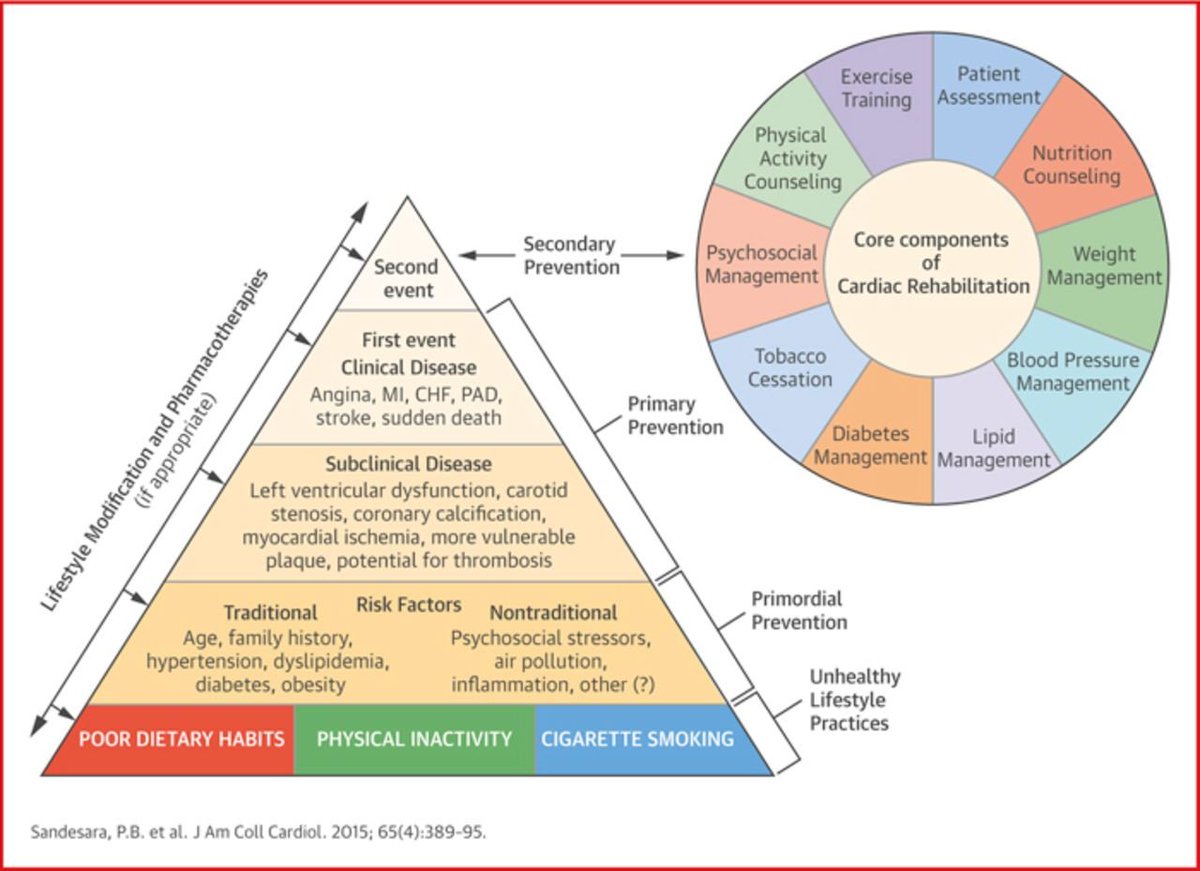
2/10 Cardiac Rehab – Secondary prevention #FITSurvivalGuide
1⃣Key Components
🚬 cessation, lipid mgmt, 🍄🍒🥥🥦🥬 counseling, ⬇️weight, 🆗blood pressure, psychosocial 🛋️, 🏋️♀️🏋️♂️⛹️♀️🏊♂️🏌️♀️🚣♂️⚽️, Diabetes mgmt
1⃣Key Components
🚬 cessation, lipid mgmt, 🍄🍒🥥🥦🥬 counseling, ⬇️weight, 🆗blood pressure, psychosocial 🛋️, 🏋️♀️🏋️♂️⛹️♀️🏊♂️🏌️♀️🚣♂️⚽️, Diabetes mgmt

3/10 Cardiac Rehab – Secondary prevention #FITSurvivalGuide
2⃣Benefits
Why? 25% mortality ⬇️, Benefit for >5yrs post-participation, ⬇️ symptoms, ⬇️ non-fatal MI for 1 year, ⬆️ 💊adherence, ⬆️ health factors, ⬇️ healthcare 💰💰.
2⃣Benefits
Why? 25% mortality ⬇️, Benefit for >5yrs post-participation, ⬇️ symptoms, ⬇️ non-fatal MI for 1 year, ⬆️ 💊adherence, ⬆️ health factors, ⬇️ healthcare 💰💰.
Evaluation of Cardiac Masses:
A Tweetorial for #FITSurvivalGuide 🚨 #ACCImaging @ASE360 @SCMR @journalofCMR @ACCinTouch
Dedicated:@dr_chirumamilla & all #ACCFIT in #CardioTwitter
Main Ref: link.springer.com/article/10.100… Palaskas, et al. Curr Treat Options Cardio Med (2018) 20: 29.
A Tweetorial for #FITSurvivalGuide 🚨 #ACCImaging @ASE360 @SCMR @journalofCMR @ACCinTouch
Dedicated:@dr_chirumamilla & all #ACCFIT in #CardioTwitter
Main Ref: link.springer.com/article/10.100… Palaskas, et al. Curr Treat Options Cardio Med (2018) 20: 29.

Usually, it all starts with an abnormal finding in an echo suggestive of intracavitary mass. How can we tell one from the other? It can be confusing. 

For artifacts, I did a Tweetorial already that describes the most common ones. Basic understanding of ultrasound physics is needed to be able to explain them: twitter.com/i/moments/1030…
Our #FITSurvivalGuide continues with antiarrhythmic drugs! (AADs)
1️⃣Basic concepts
2️⃣Classification
3️⃣Class 1(a/b/c)
4️⃣Class 3
5️⃣Amio/dronedarone
6️⃣Clinical use
7️⃣Pearls and pitfalls
1️⃣Basic concepts
2️⃣Classification
3️⃣Class 1(a/b/c)
4️⃣Class 3
5️⃣Amio/dronedarone
6️⃣Clinical use
7️⃣Pearls and pitfalls

1️⃣ Arrhythmias originate from ectopy +/- reentry.
AADs work by:
*⬇️ing ectopy
*⬆️ing refractoriness (⬇️ing reentry)
AADs work by:
*⬇️ing ectopy
*⬆️ing refractoriness (⬇️ing reentry)
2️⃣
Class1: sodium channel blockers
(⬇️ ectopy, ⬇️ reentry by raising threshold for cell-cell conduction)
C2: beta blockers
C3: potassium channel blockers
(⬆️ action potential, ⬆️ AP "wavelength", ⬇️ excitable gap for reentry)
C4: calcium channel blockers
Class1: sodium channel blockers
(⬇️ ectopy, ⬇️ reentry by raising threshold for cell-cell conduction)
C2: beta blockers
C3: potassium channel blockers
(⬆️ action potential, ⬆️ AP "wavelength", ⬇️ excitable gap for reentry)
C4: calcium channel blockers
1/11
A #tweetorial on Syncope #FITsurvivalguide
Definition:
Sudden transient loss of consciousness with associated loss of postural tone, spontaneous recovery without neurologic deficits
The key is in the H&P
A good H&P can provide a dx in up to 50% of cases.

A #tweetorial on Syncope #FITsurvivalguide
Definition:
Sudden transient loss of consciousness with associated loss of postural tone, spontaneous recovery without neurologic deficits
The key is in the H&P
A good H&P can provide a dx in up to 50% of cases.
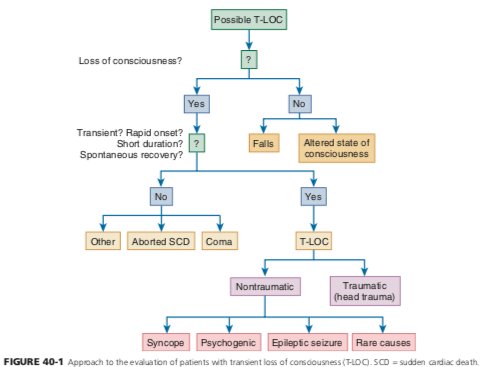

2
Goals.
1. Determine specific cause; this will direct therapy, prevent recurrences, ⬇️ expensive evaluations, and improve outcome.
2. Determine presence of cardiac syncope which portends ⬆️ mortality and sudden death.
3. Identify those who will benefit Inpt 🆚 outpt eval
Goals.
1. Determine specific cause; this will direct therapy, prevent recurrences, ⬇️ expensive evaluations, and improve outcome.
2. Determine presence of cardiac syncope which portends ⬆️ mortality and sudden death.
3. Identify those who will benefit Inpt 🆚 outpt eval
A #tweetorial on Perioperative risk assessment for Non-cardiac surgeries for #FITsurvivalguide
⚠️NOT "clearance"!
Purpose of consult
-Evaluate pt`s medical status
-Risk assessment
-Management recs
-Treat modifiable risk factors
-"Team" approach for shared decision making
⚠️NOT "clearance"!
Purpose of consult
-Evaluate pt`s medical status
-Risk assessment
-Management recs
-Treat modifiable risk factors
-"Team" approach for shared decision making
2/ Triggers for perioperative myocardial injury
-Inflammatory state
-Hypercoagulable state
-Stress state
-Hypoxic state
All predispose to ischemia and coronary thrombosis.
-Inflammatory state
-Hypercoagulable state
-Stress state
-Hypoxic state
All predispose to ischemia and coronary thrombosis.
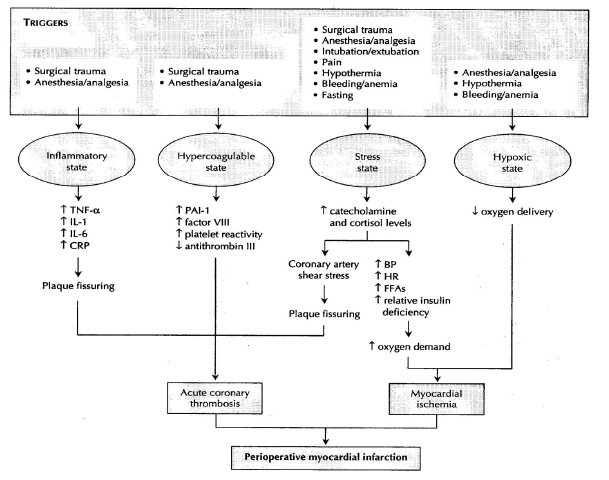
3/ Think about- 🤔
-Should pt have surgery? Emergent or not?
-Type of surgery and type of anesthesia?
-Functional status of the pt?
-Relevant medical hx and any ongoing cardiac sx?
-Review the meds.
-Prior cardiac w/u.
Focus on good history and PE, can save a lot of tests & 💸
-Should pt have surgery? Emergent or not?
-Type of surgery and type of anesthesia?
-Functional status of the pt?
-Relevant medical hx and any ongoing cardiac sx?
-Review the meds.
-Prior cardiac w/u.
Focus on good history and PE, can save a lot of tests & 💸
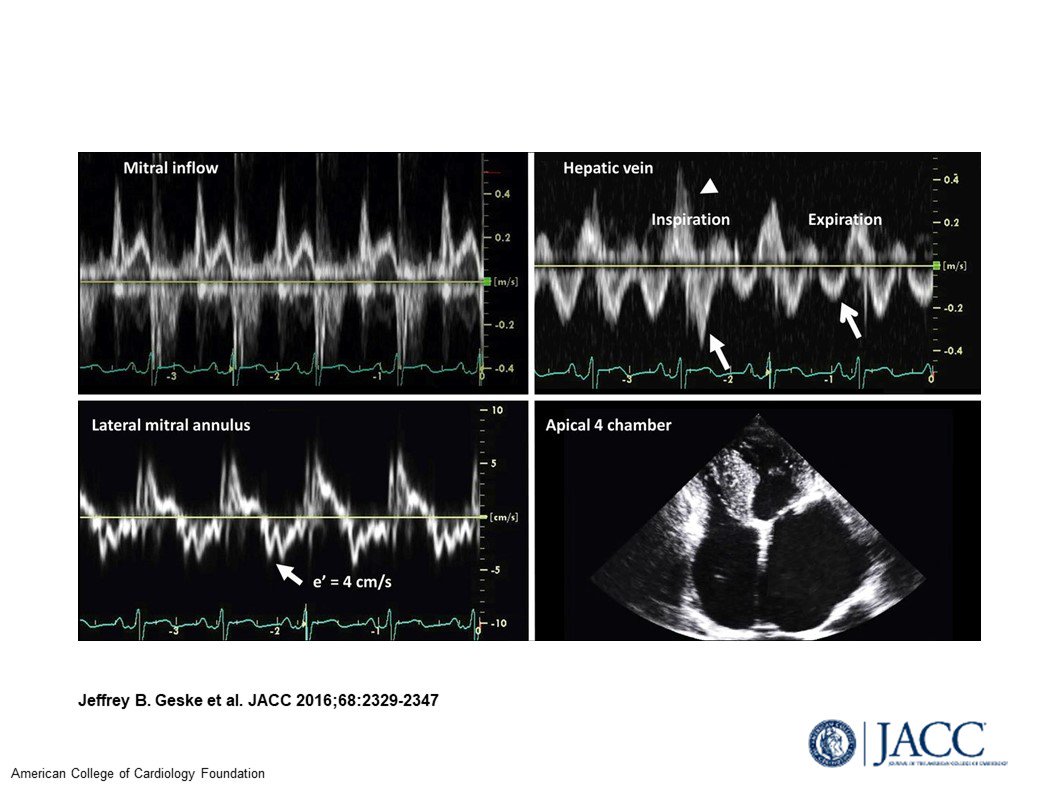
#FITSurvivalGuide on Restrictive Cardiomyopathy (RCM) vs Constrictive Pericarditis (CP).
In both:
💠Diastolic RV & LV impaired; systolic function preserved
💠HFpEF phenotype, predominant “R sided” signs (JVP, edema, ascites)
1/12
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD
In both:
💠Diastolic RV & LV impaired; systolic function preserved
💠HFpEF phenotype, predominant “R sided” signs (JVP, edema, ascites)
1/12
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD
🔑 to understanding different filling:
RCM = myocardial disorder
CP = pericardial disorder.
2/12
@majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @sabeedak1 @noshreza @SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @drjohnm @heartdoc45 @zainasadEP @docaward
RCM = myocardial disorder
CP = pericardial disorder.
2/12
@majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @sabeedak1 @noshreza @SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @drjohnm @heartdoc45 @zainasadEP @docaward
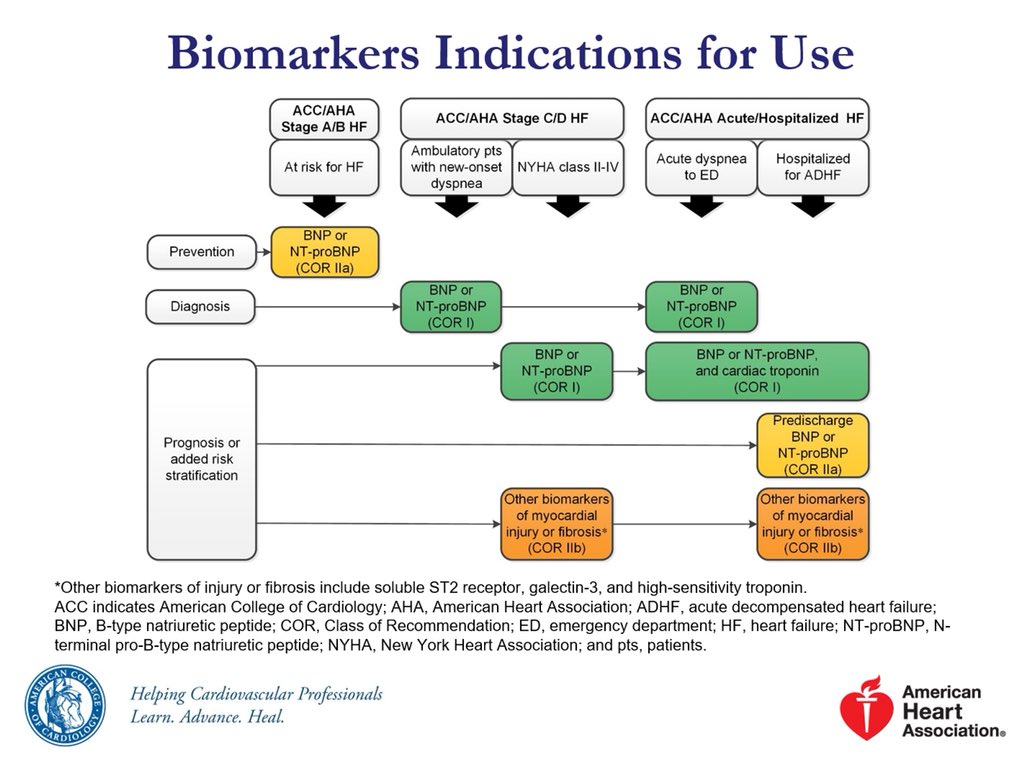
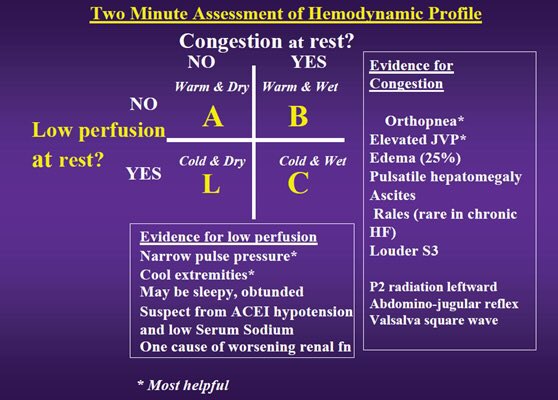
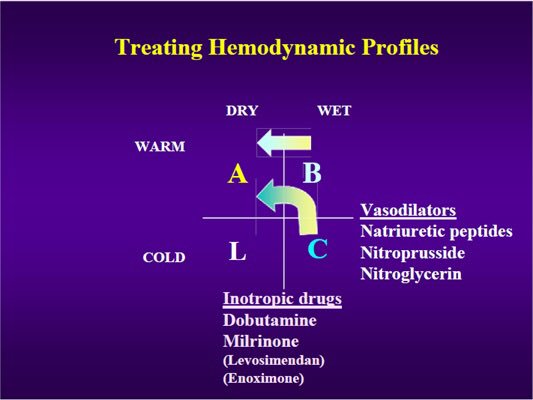
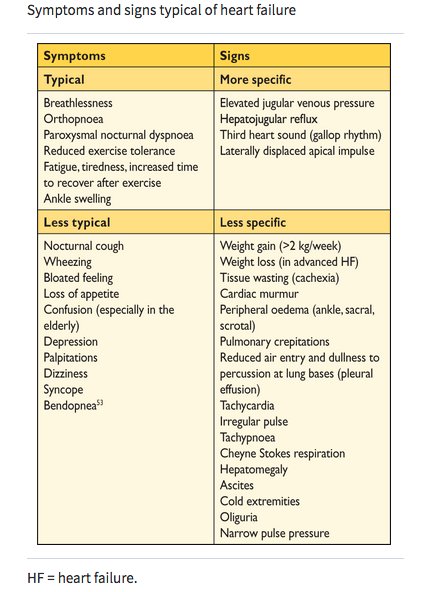
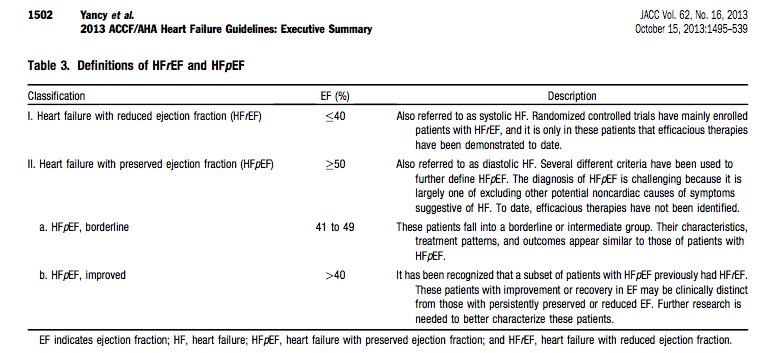
#FITSurvivalGuide: #HeartFailure management — a #tweetorial for #ACCFIT
1️⃣ Non-pharmacologic
2️⃣ Acute HF
3️⃣ Staging
4️⃣ HFrEF
5️⃣ HFpEF
6️⃣ Devices
7️⃣ Advanced Tx
8️⃣ Misc
Resources: @HFSA @ishlt @AHAScience @JACCJournals @HRSonline
1️⃣ Non-pharmacologic
2️⃣ Acute HF
3️⃣ Staging
4️⃣ HFrEF
5️⃣ HFpEF
6️⃣ Devices
7️⃣ Advanced Tx
8️⃣ Misc
Resources: @HFSA @ishlt @AHAScience @JACCJournals @HRSonline
#FITSurvivalGuide #tweetorial Diagnosis of Heart failure: HF is a complex clinical syndrome related to structural or functional impairment of ventricular filling or contraction. HF can be classified into HFrEF and HFpEF based on assessment of LVEF. 
My #FITSurvivalGuide Tweetorial on the Dx/Rx of wide complex tachycardia: SVT vs VT
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD @majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @mmamas1973 @CMichaelGibson @DocSavageTJU @rajivxgulati @SVRaoMD @MinnowWalsh
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD @majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @mmamas1973 @CMichaelGibson @DocSavageTJU @rajivxgulati @SVRaoMD @MinnowWalsh
Step 1 w WCT is to assess ABCs. If the pt is unstable or in shock, it doesn't matter what the rhythm is> just shock the patient #FITSurvivalGuide
@sabeedak1 @noshreza @chadialraies @mirvatalasnag @venkmurthy @fischman_david i @vietheartPA @DrKevinCampbell @krishmd @cardiodee
@sabeedak1 @noshreza @chadialraies @mirvatalasnag @venkmurthy @fischman_david i @vietheartPA @DrKevinCampbell @krishmd @cardiodee
Step 2 for WCT is stop and think. Engage Kahneman's System 2 brain. Embrace Lord Bayes' concept of priors
What are the three reasons a tachy becomes wide?
#FITSurvivalGuide
@SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @heartdoc45 @zainasadEP @docaward @yogitar @KevinShahMD
What are the three reasons a tachy becomes wide?
#FITSurvivalGuide
@SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @heartdoc45 @zainasadEP @docaward @yogitar @KevinShahMD
#FITSurvivalGuide #ACCFIT
Topic - Ventricular Tachycardia!
Agenda:
1- Approach to evaluating #VT
2- Management of #VT
3- Practice Cases
Please share your thoughts & input to this #tweetorial!
@ACCCardioEd @ACCinTouch #FOAMed @MichiganACC

Topic - Ventricular Tachycardia!
Agenda:
1- Approach to evaluating #VT
2- Management of #VT
3- Practice Cases
Please share your thoughts & input to this #tweetorial!
@ACCCardioEd @ACCinTouch #FOAMed @MichiganACC
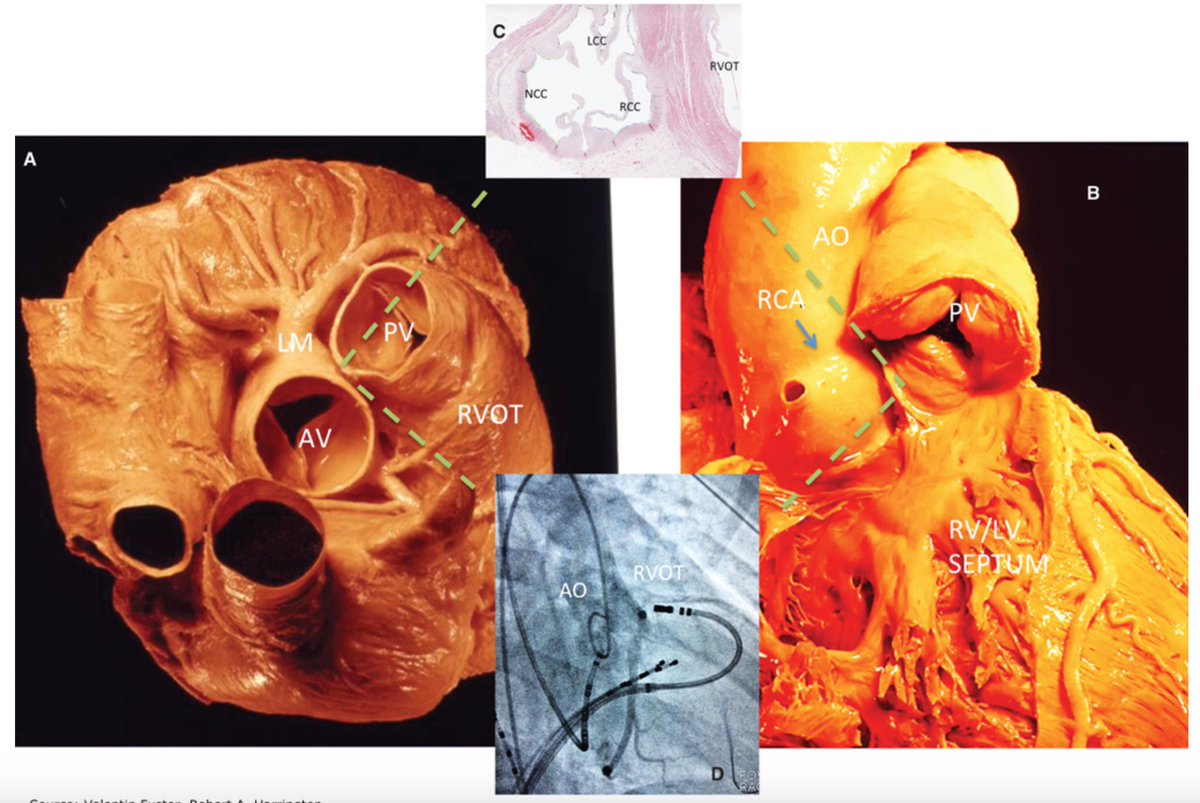
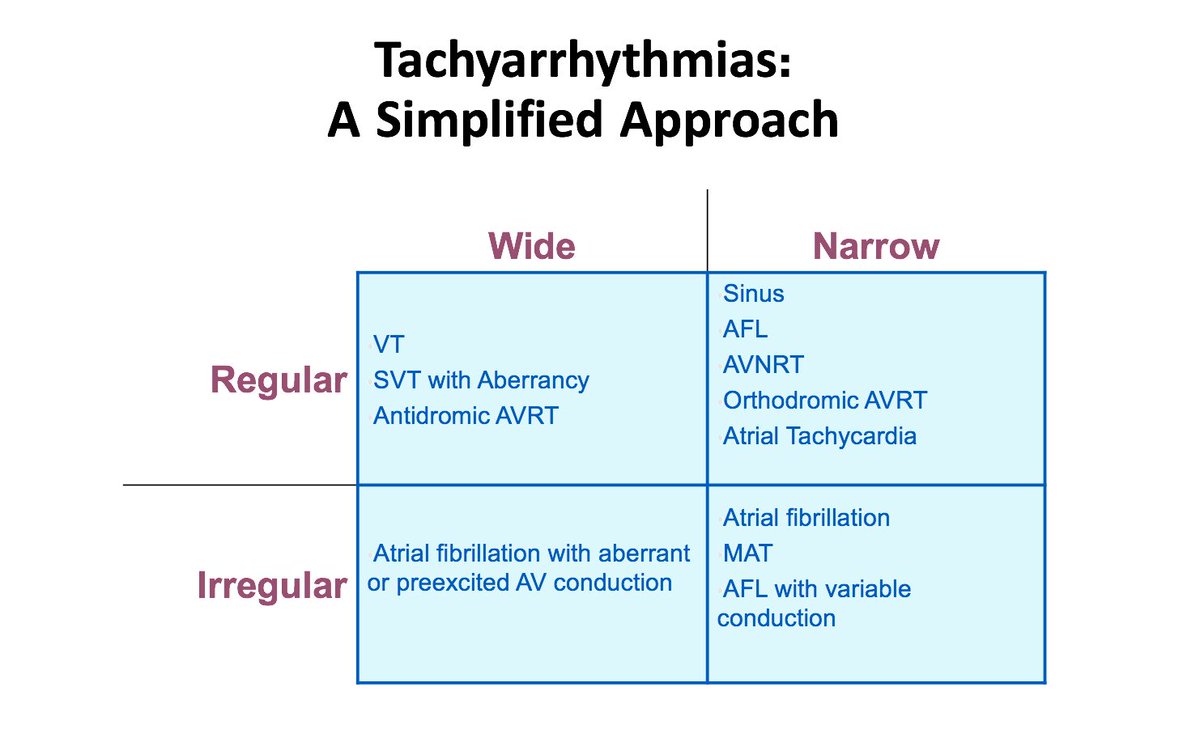
#FITSurvivalGuide #ACCFIT
1/10 – Ventricular Tachycardia
Simplified approach to evaluate tachycardia:
Rule #1 – If HD unstable ➡️ shock!
If HD stable, sit down & think.
Step # 1 - QRS: wide or narrow?
Step # 2 - Rhythm: regular or irregular?
This will narrow DDx!
1/10 – Ventricular Tachycardia
Simplified approach to evaluate tachycardia:
Rule #1 – If HD unstable ➡️ shock!
If HD stable, sit down & think.
Step # 1 - QRS: wide or narrow?
Step # 2 - Rhythm: regular or irregular?
This will narrow DDx!
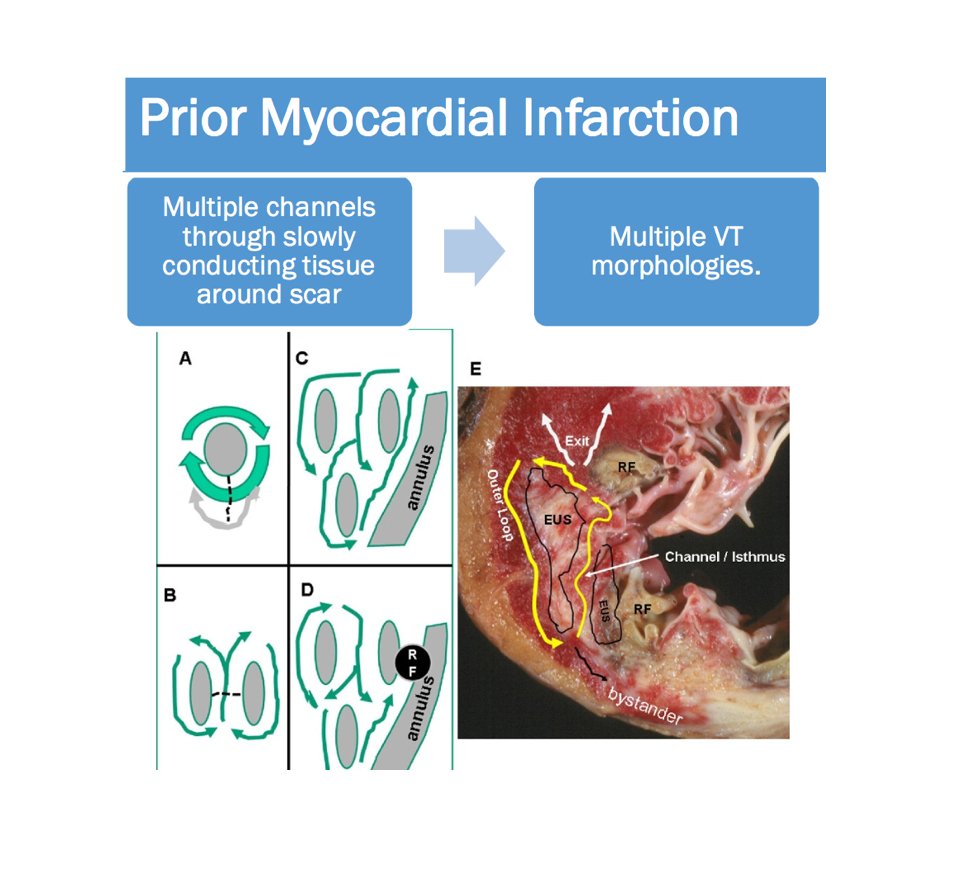
#FITSurvivalGuide #ACCFIT
2/10 - Wide complex tachycardia
Always consider clinical Scenario!
Look for history of MI and cardiomyopathy ➡️ strongly favor #VT!
* If structural heart disease is present, you will be correct 9/10 times with diagnosis of VT!
2/10 - Wide complex tachycardia
Always consider clinical Scenario!
Look for history of MI and cardiomyopathy ➡️ strongly favor #VT!
* If structural heart disease is present, you will be correct 9/10 times with diagnosis of VT!
#FITSurvivalGuide #ACCFIT
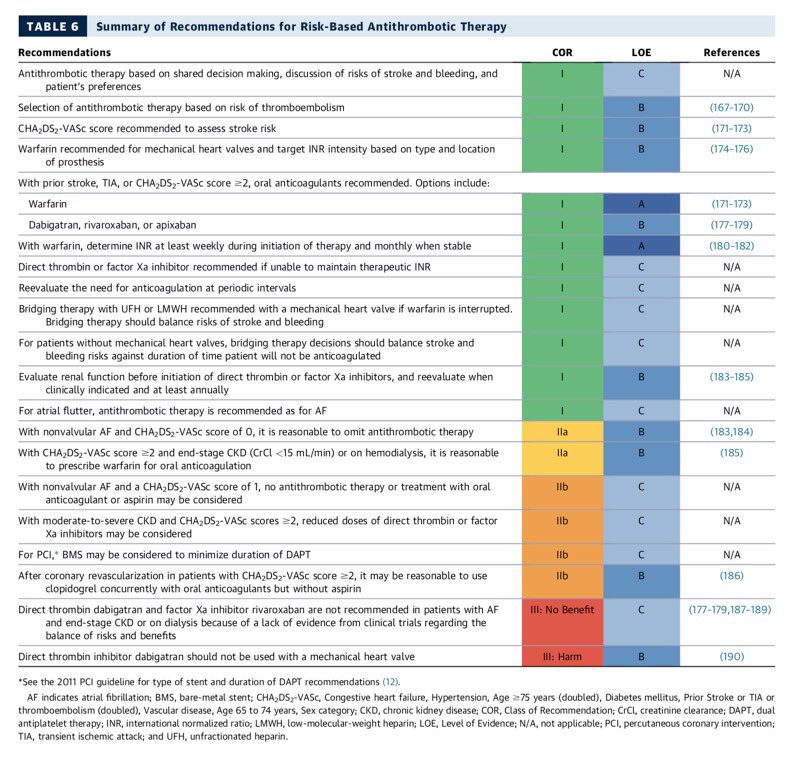
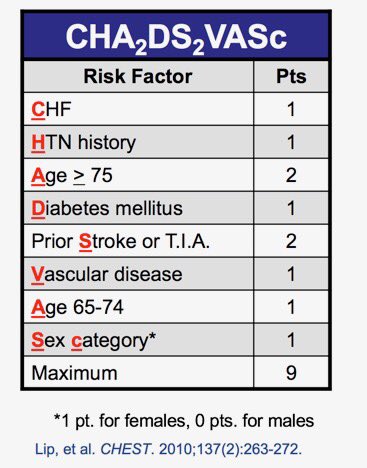
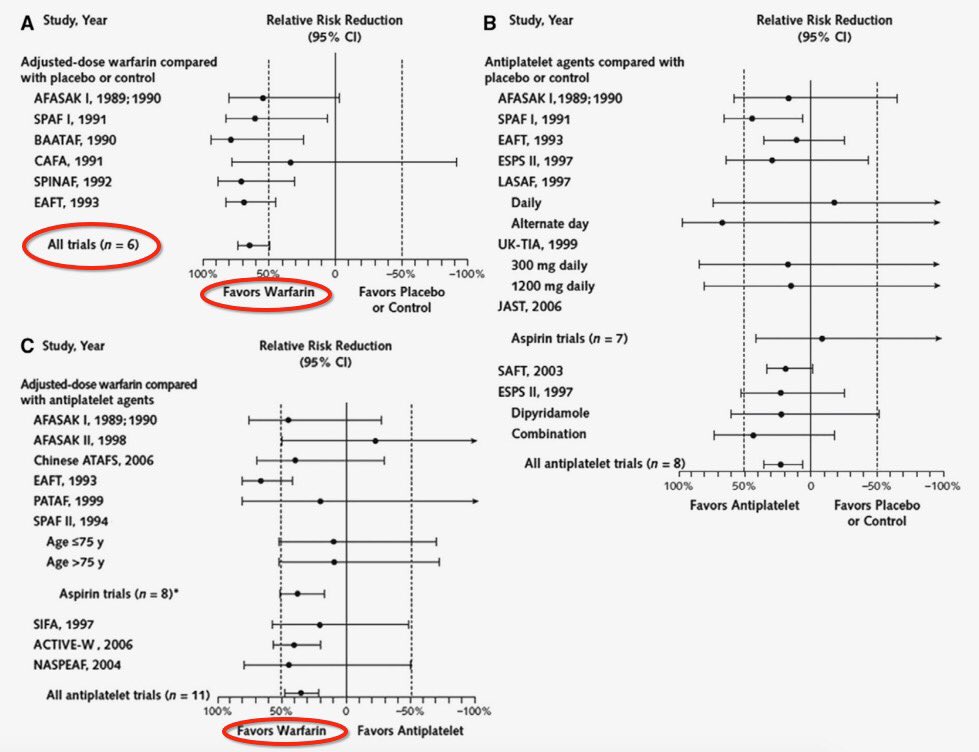
1/10: Stroke🧠 prevention in afib. #warfarin, #noacs, & LAA occlusion devices.
◽️shared decision making is key 🔑
◽️CHADS-Vasc to stratify risk
◽️factor 💸and CrCl 🚽
◽️DAPT+AC= ↑↑bleeding




1/10: Stroke🧠 prevention in afib. #warfarin, #noacs, & LAA occlusion devices.
◽️shared decision making is key 🔑
◽️CHADS-Vasc to stratify risk
◽️factor 💸and CrCl 🚽
◽️DAPT+AC= ↑↑bleeding

2/10
For a quick review on coagulation physiology as it pertains to AC see 📽below.
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD @majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @sabeedak1 @noshreza
@SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @drjohnm
For a quick review on coagulation physiology as it pertains to AC see 📽below.
@dr_chirumamilla @Pooh_Velagapudi @bcostelloMD @majazayeri @fawazalenezi55 @SanChris999 @GuruKowlgi @Nidhi_Madan9 @sabeedak1 @noshreza
@SaggerMawri @nsivcd @DrManiCardio @khandelwalMD @drjohnm
3/10
Warfarin 🐀☣️
◽️interferes with normal post translational gamma-carboxylation of vitamin K dependent clotting factors 2️⃣7️⃣9️⃣🔟
◽️doesn’t inactivate functional clotting factors
◽️prothrombin half life: 72h
◽️Ergo INR effect 24-36 hr
🛑 teratogenic
Warfarin 🐀☣️
◽️interferes with normal post translational gamma-carboxylation of vitamin K dependent clotting factors 2️⃣7️⃣9️⃣🔟
◽️doesn’t inactivate functional clotting factors
◽️prothrombin half life: 72h
◽️Ergo INR effect 24-36 hr
🛑 teratogenic
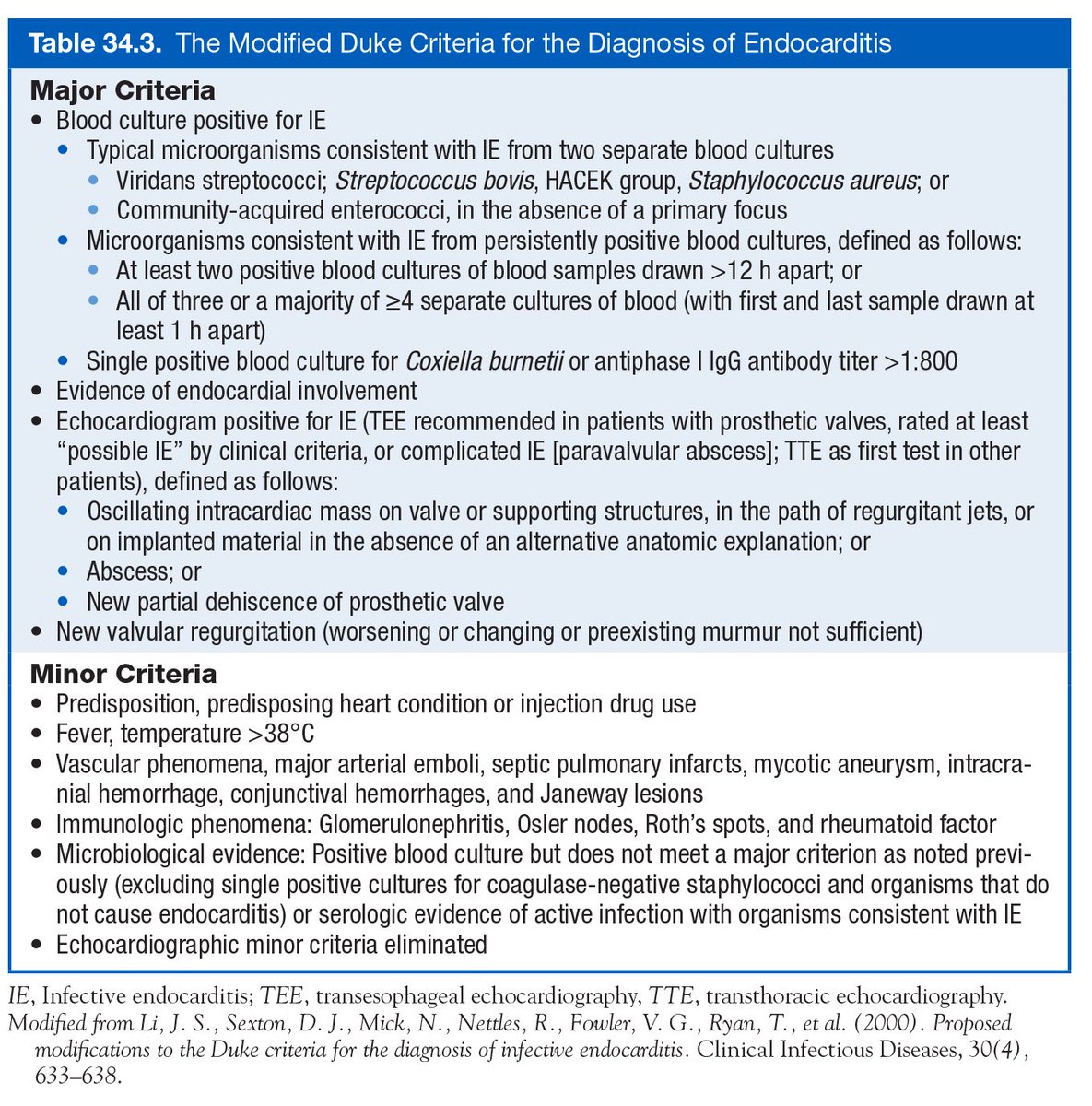
#FITSurvivalGuide #ACCFIT
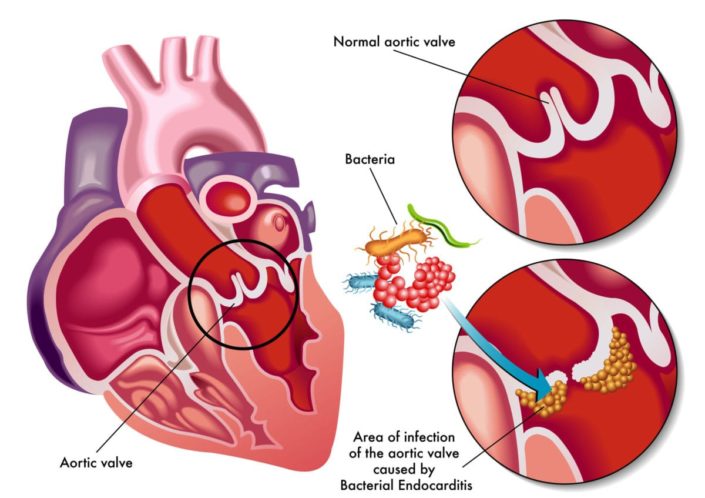
#InfectiveEndocarditis.
1/10 Not comprehensive. ⬇️⬇️some imp. points. Hx, exam, echo, micro data essential to diagnose & treat apporpriately. Suggested read : 2014 ACC/AHA valve guideline with 2017 Focused update.
cc: @dr_chirumamilla


#InfectiveEndocarditis.
1/10 Not comprehensive. ⬇️⬇️some imp. points. Hx, exam, echo, micro data essential to diagnose & treat apporpriately. Suggested read : 2014 ACC/AHA valve guideline with 2017 Focused update.
cc: @dr_chirumamilla
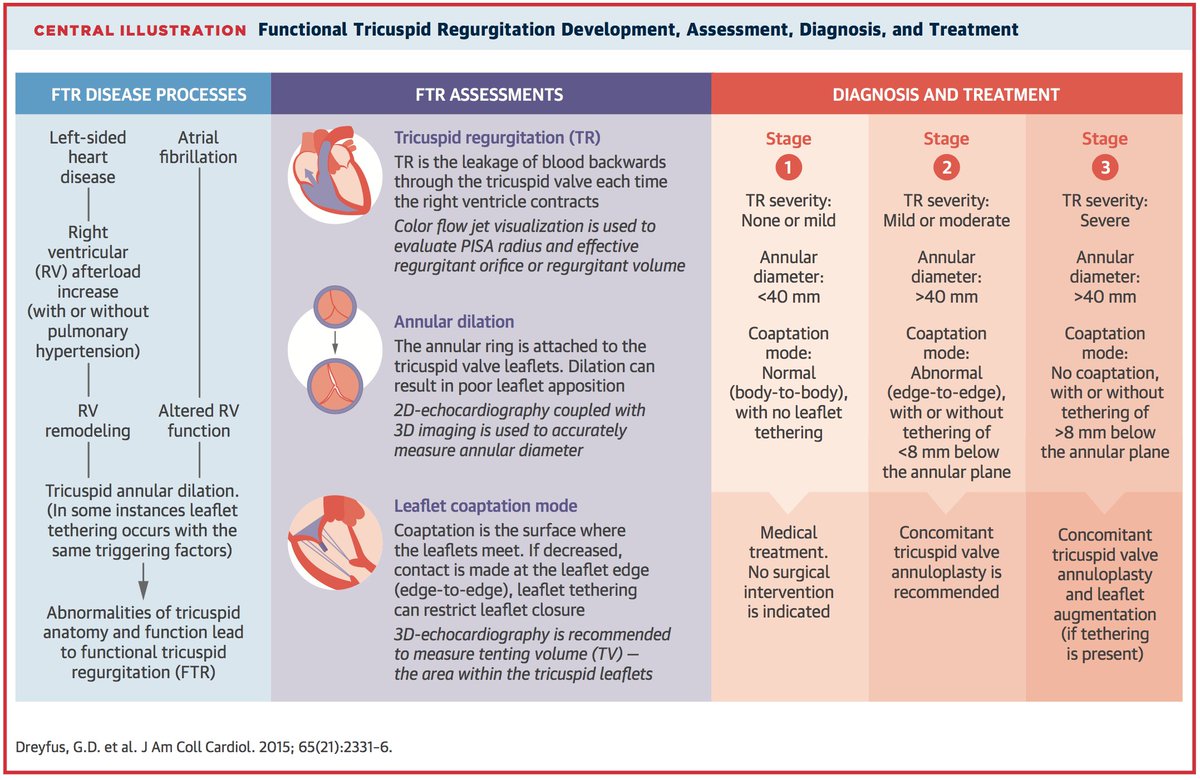
#FITSurvivalGuide: The Forgotten Valve-#TricuspidRegurgitation (#TR) #tweetorial for the new #ACCFIT!
1⃣ Anatomy
2⃣ Etiologies
3⃣ Classification
4⃣ Diagnosis
5⃣ Treatment
Resources: @ASE360 @JACCJournals @CircAHA @ACCCardioEd @UMNews @Medtronic
1/10
cc: @dr_chirumamilla
1⃣ Anatomy
2⃣ Etiologies
3⃣ Classification
4⃣ Diagnosis
5⃣ Treatment
Resources: @ASE360 @JACCJournals @CircAHA @ACCCardioEd @UMNews @Medtronic
1/10
cc: @dr_chirumamilla
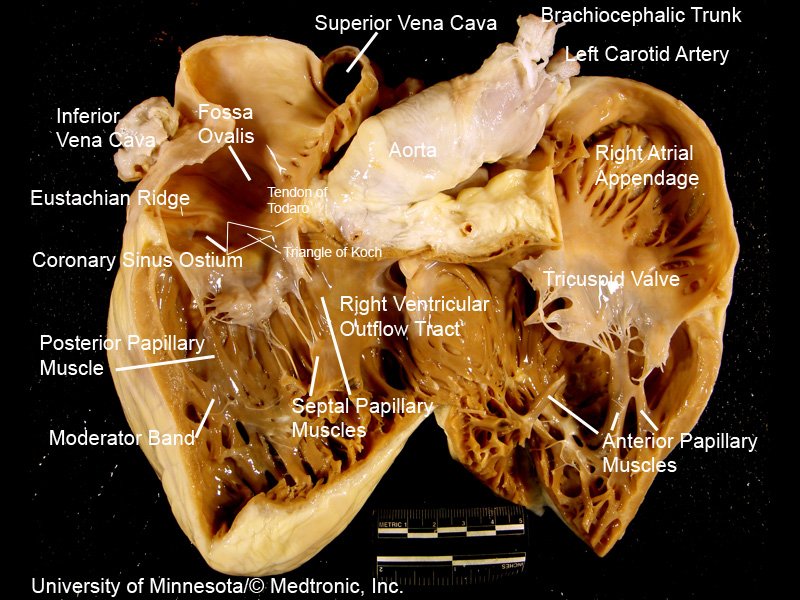
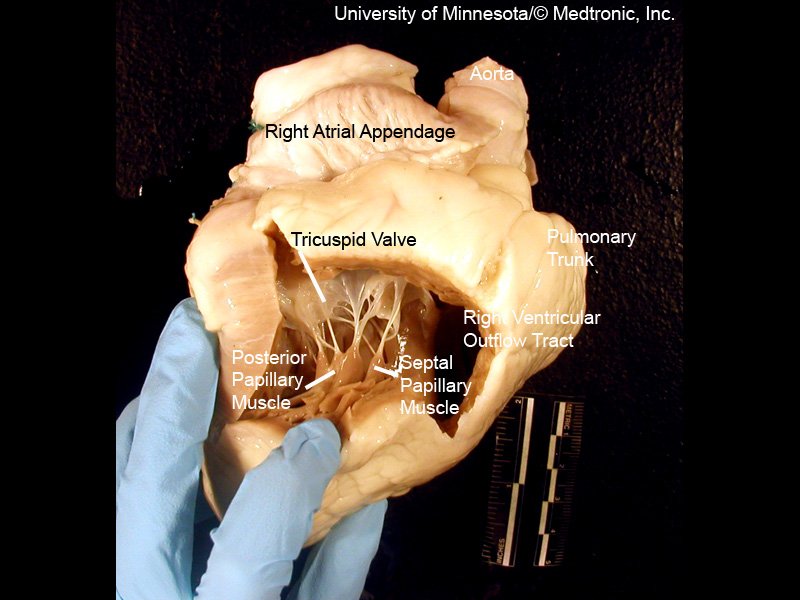
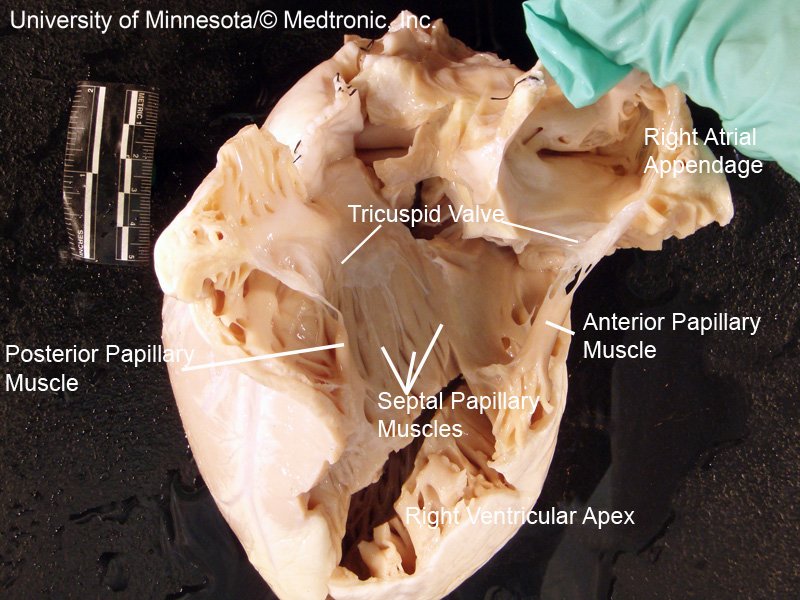
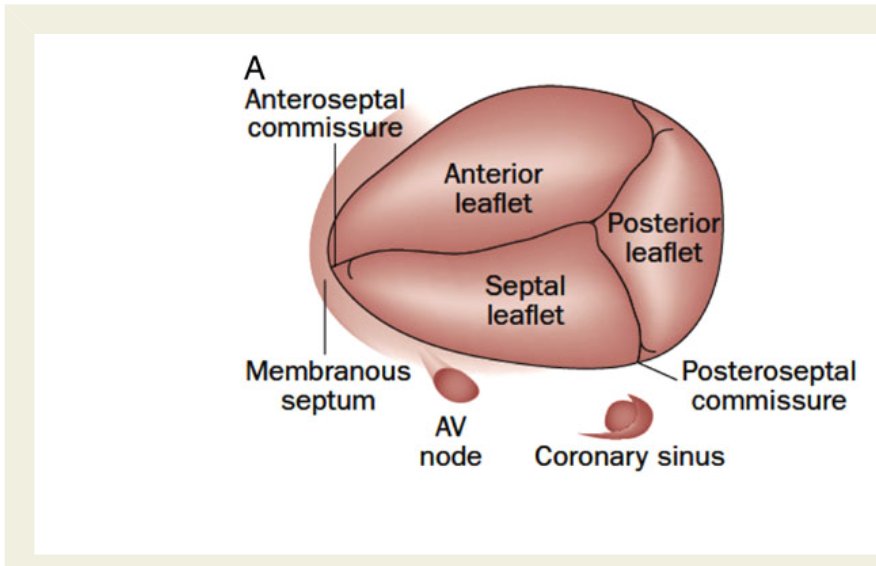
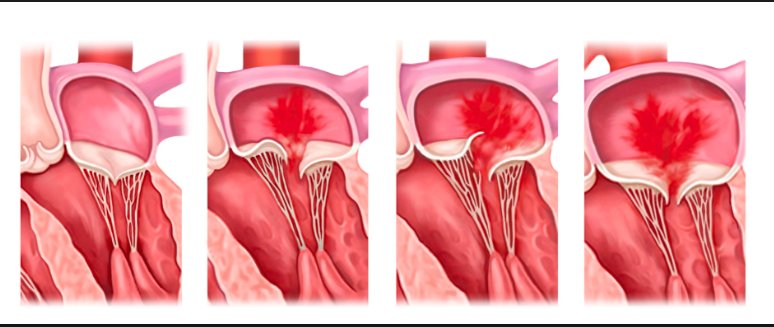
[2/10] Impt to understand #TricuspidValve 1⃣ Anatomy
3 leaflets ⬇️ + fibrous annulus + 2 papillary 💪🏽 + chordae tendinae + RA/RV ❤️
⬛️ Anterior 🍃 (largest)
◾️Posterior
▪️Septal (smallest)
(note: throughout #tweetorial, see image descriptions for more content)



3 leaflets ⬇️ + fibrous annulus + 2 papillary 💪🏽 + chordae tendinae + RA/RV ❤️
⬛️ Anterior 🍃 (largest)
◾️Posterior
▪️Septal (smallest)
(note: throughout #tweetorial, see image descriptions for more content)
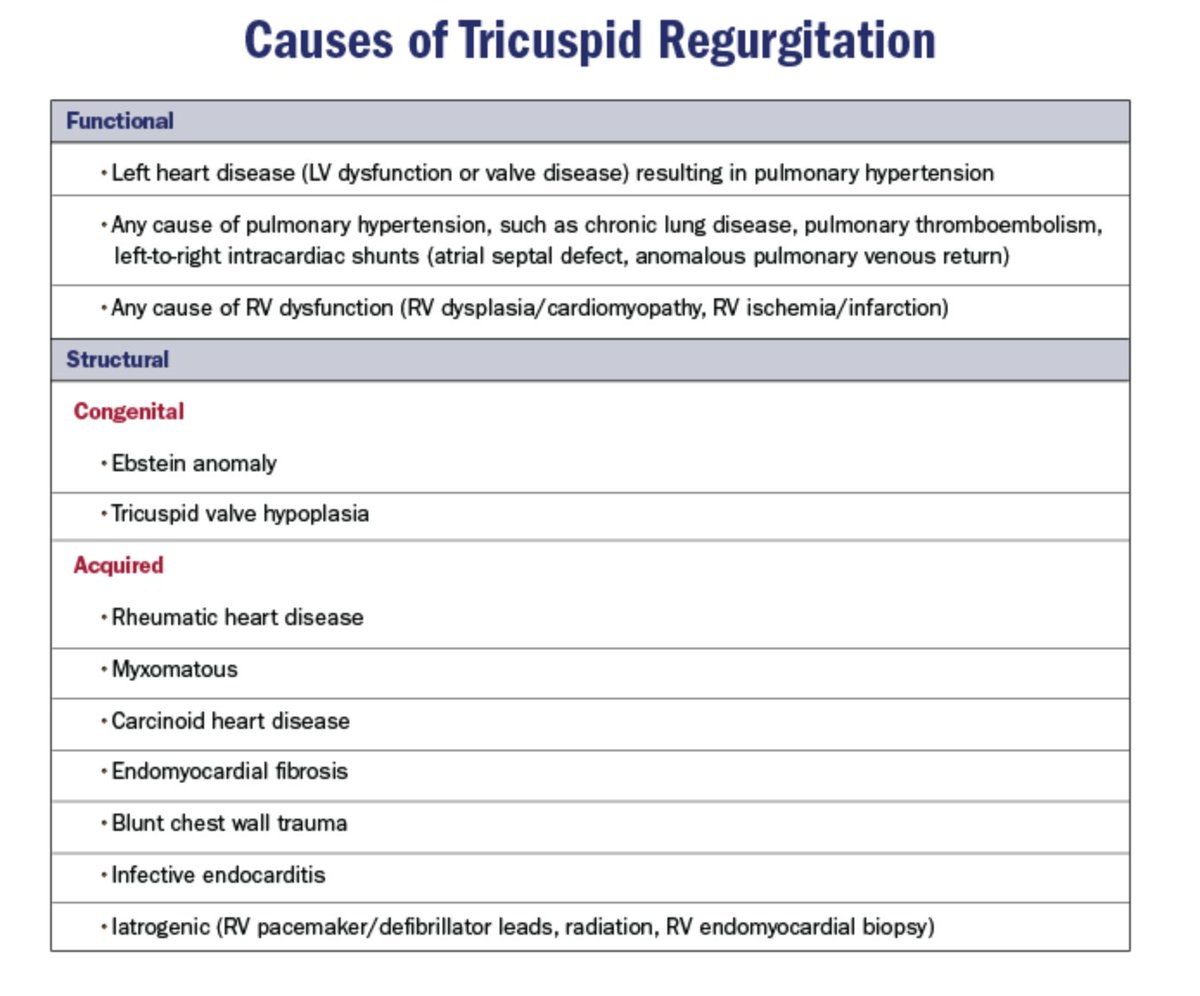
[3/10] 2⃣ Etiologies = Structural (1º) vs. Functional (FTR)
Keep chart ⬇️ DDx in mind when reading #EchoFirst
~80% of significant TR = FTR/2º to TA dilatation + leaflet tethering ⬅️ RV remodeling ⬅️ volume and/or pressure overload
Structural (1º) cause = less common

Keep chart ⬇️ DDx in mind when reading #EchoFirst
~80% of significant TR = FTR/2º to TA dilatation + leaflet tethering ⬅️ RV remodeling ⬅️ volume and/or pressure overload
Structural (1º) cause = less common
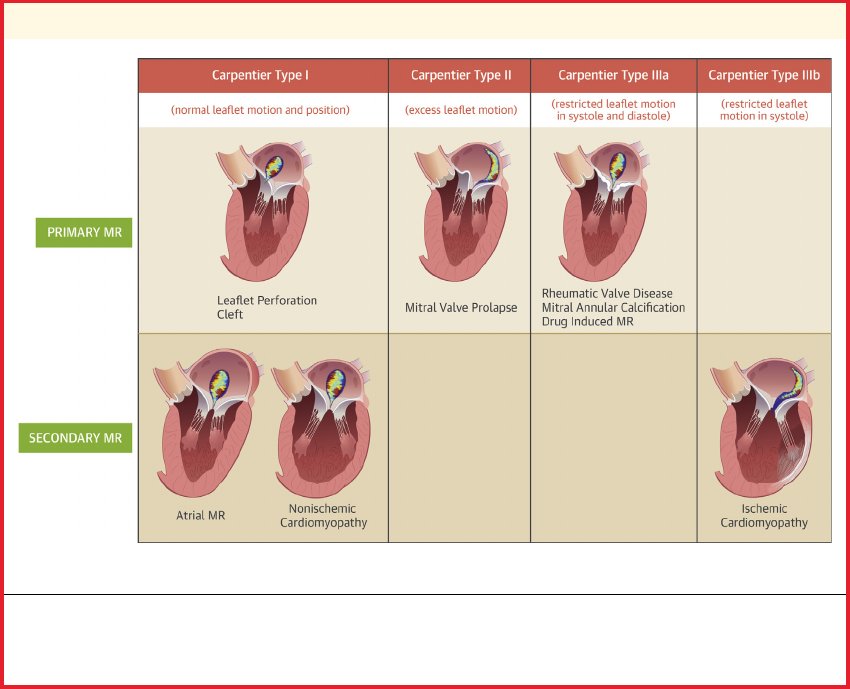
Continuing #FITSurvivalGuide: Brief outlook Mitral Regurgitation (MR) Management
(awesome part 1 of MR dx by @sairasamani)
⬆️age = ⬆️incident MR requiring ?🏥zations/intervention -->healthcare 💰💰
Untreated severe MR ass. w/ poor outcomes 2/2 volume overload of the ❤️
(awesome part 1 of MR dx by @sairasamani)
⬆️age = ⬆️incident MR requiring ?🏥zations/intervention -->healthcare 💰💰
Untreated severe MR ass. w/ poor outcomes 2/2 volume overload of the ❤️
#FITSurvivalGuide 1/10 Tweetorial on MR. From JASE April 2017. This is an extensive topic, and a tweetorial will not do justice, so highly recommend to read this article. @ASE360 @ACCCardioEd @newmexicoacc #echoboards 

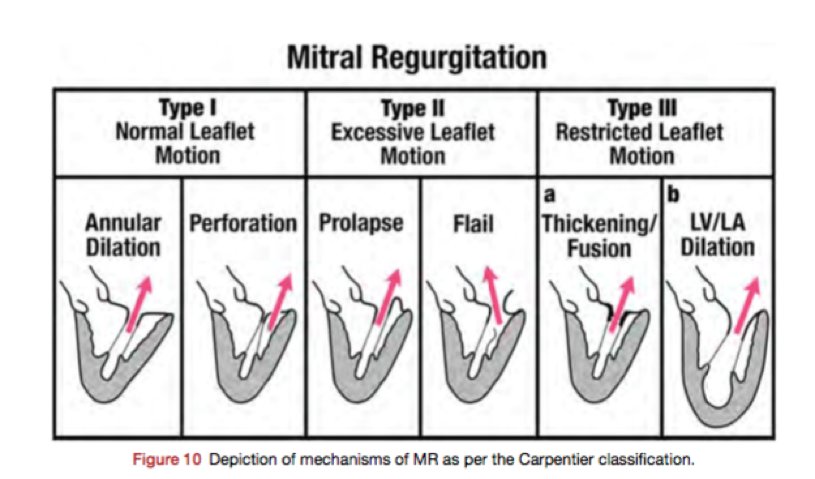
2/10
MR can be 1’ or 2’. Simplified version: 1’ MR d/t pathology of the valve itself. 2’ MR = MV apparatus is intact, w/ ventricular disease (LV dilatation) dilated MV annulus to MV leaflets malcoaptation MR (~central jet). Also useful to use Carpentier classification.
MR can be 1’ or 2’. Simplified version: 1’ MR d/t pathology of the valve itself. 2’ MR = MV apparatus is intact, w/ ventricular disease (LV dilatation) dilated MV annulus to MV leaflets malcoaptation MR (~central jet). Also useful to use Carpentier classification.
3/10
Determine the scallops. First heard from @MayoClinicCV: 2 steps
1.At 0 deg: Determine if ant or post leaflet abn
2.At 60 deg: Determine which scallop 1,2, or 3
Pic from J Am Soc Echocardiogr 2013;26:921-64
Determine the scallops. First heard from @MayoClinicCV: 2 steps
1.At 0 deg: Determine if ant or post leaflet abn
2.At 60 deg: Determine which scallop 1,2, or 3
Pic from J Am Soc Echocardiogr 2013;26:921-64

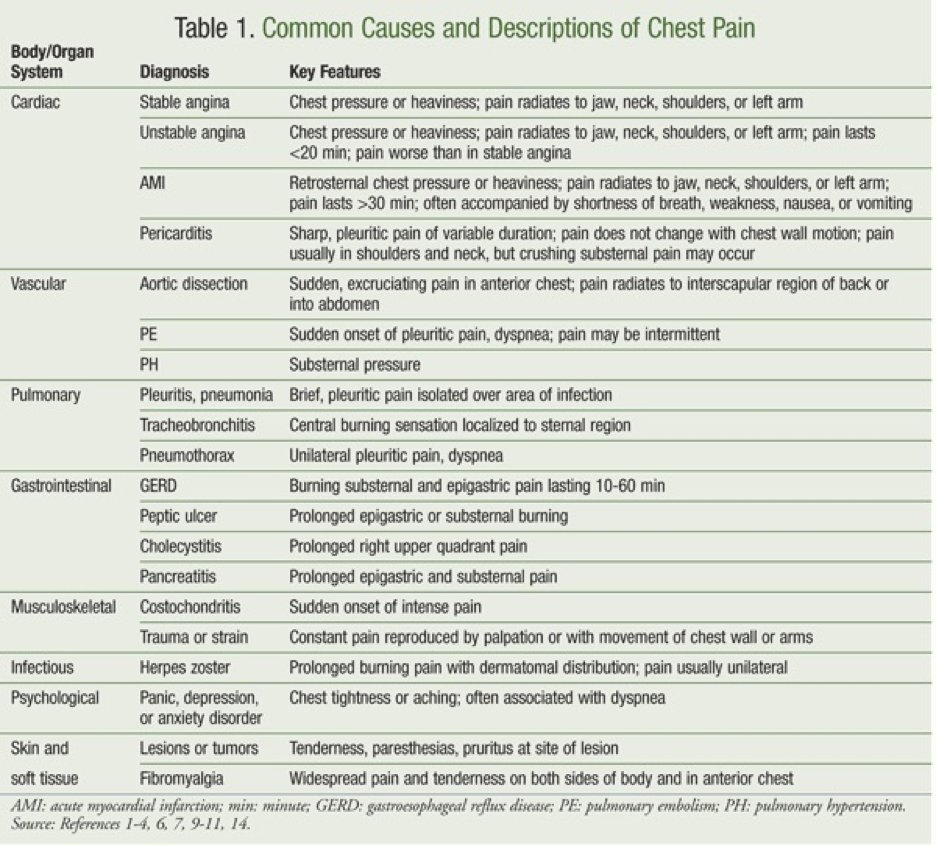
1/10 What is chest pain? #FITSurvivalGuide #Tweetorial
- "Pain anywhere in the chest" 🤦♀️
- Many things cause chest pain
- ❤️ vs ❌❤️
- ❤️ - ischemic vs non ischemic
- Life threatening vs not
- "Pain anywhere in the chest" 🤦♀️
- Many things cause chest pain
- ❤️ vs ❌❤️
- ❤️ - ischemic vs non ischemic
- Life threatening vs not
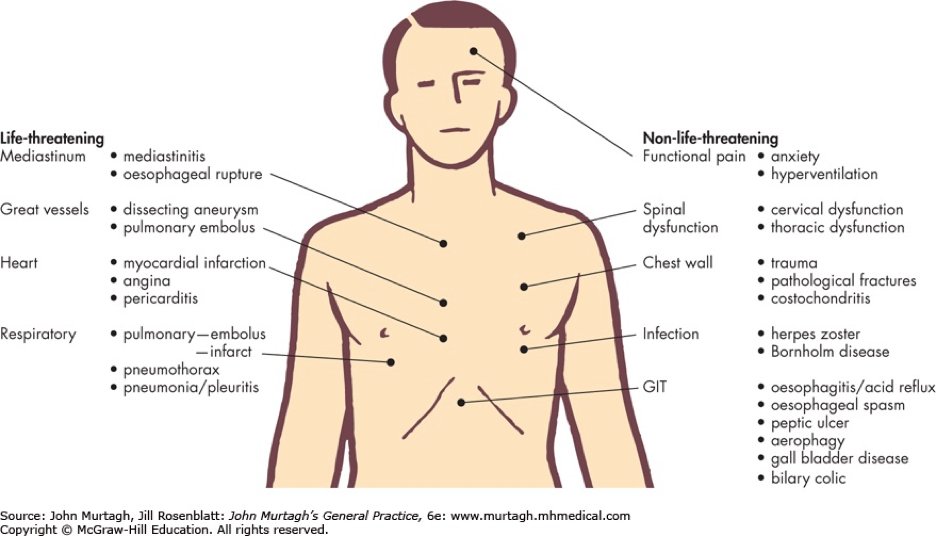
2/10 - Common causes of chest pain (by system) #FITSurvivalGuide
- Cardiac
- Pulmonary
- GI
- MSK
- Infectious
- Psych
- Skin/ soft tissue
- Cardiac
- Pulmonary
- GI
- MSK
- Infectious
- Psych
- Skin/ soft tissue
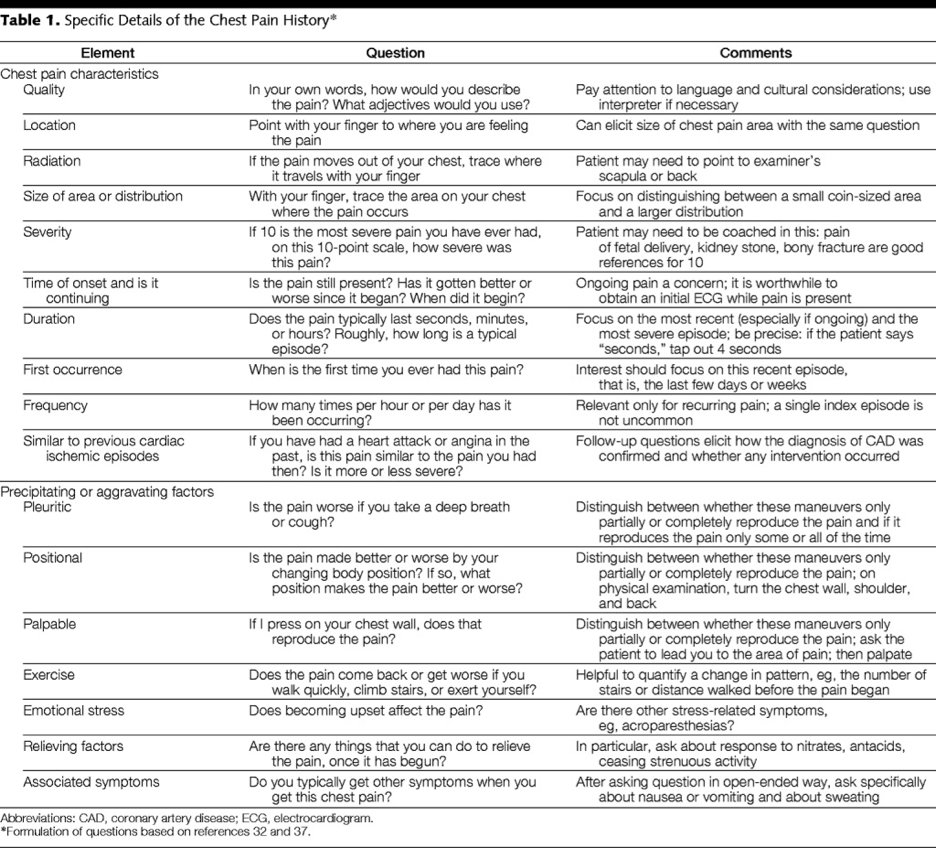
3/10 Chest pain- The History! #FITSurvivalGuide
- Going back to medical school 👩⚕️👨⚕️🥼😷
- The key to figuring out what type of chest pain the patient has!
- Quality, location, radiation, duration, associated symptoms, relieving factors!
- Going back to medical school 👩⚕️👨⚕️🥼😷
- The key to figuring out what type of chest pain the patient has!
- Quality, location, radiation, duration, associated symptoms, relieving factors!
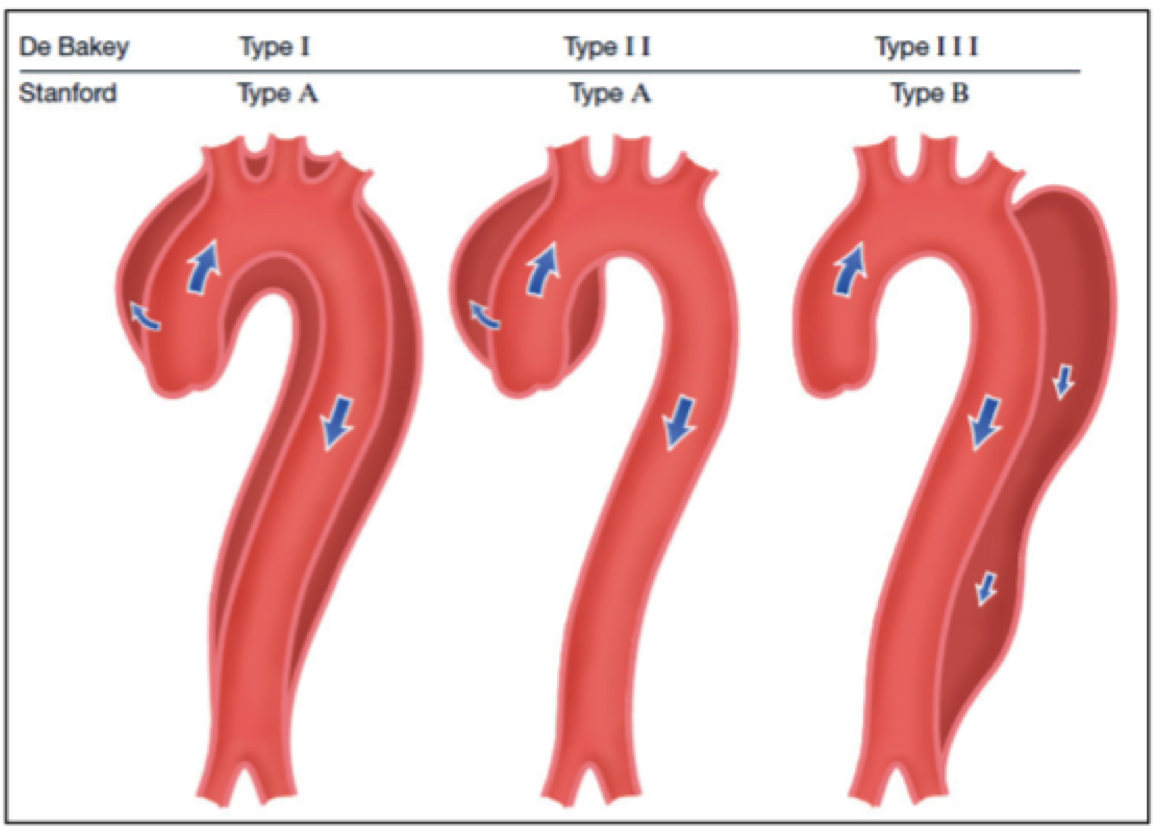
#FITSurvivalGuide Aortic Emergency style!
Will discuss presentation/dx/complications/tx for:
1. Aortic dissection💉
2. IMH❣️
3. PAU
4. Traumatic transection
5. Non-emergent aneurysm surgical cutoffs (because boards loves them!)
Hoping @keaglemd can share his expertise as well!
Will discuss presentation/dx/complications/tx for:
1. Aortic dissection💉
2. IMH❣️
3. PAU
4. Traumatic transection
5. Non-emergent aneurysm surgical cutoffs (because boards loves them!)
Hoping @keaglemd can share his expertise as well!
Everyone please feel free to add to this thread for more learning #FIT #CardioEd
@dr_chirumamilla @APostalian @heartdoc45 @Babar_Basir @DrJayMohan @SamRRazaMD @DocStrom @DocSavageTJU @SamRRazaMD @DrQuinnCapers4 @cardiojaydoc02 @DrSheilaSahni @saraceciliamtz @onco_cardiology
@dr_chirumamilla @APostalian @heartdoc45 @Babar_Basir @DrJayMohan @SamRRazaMD @DocStrom @DocSavageTJU @SamRRazaMD @DrQuinnCapers4 @cardiojaydoc02 @DrSheilaSahni @saraceciliamtz @onco_cardiology
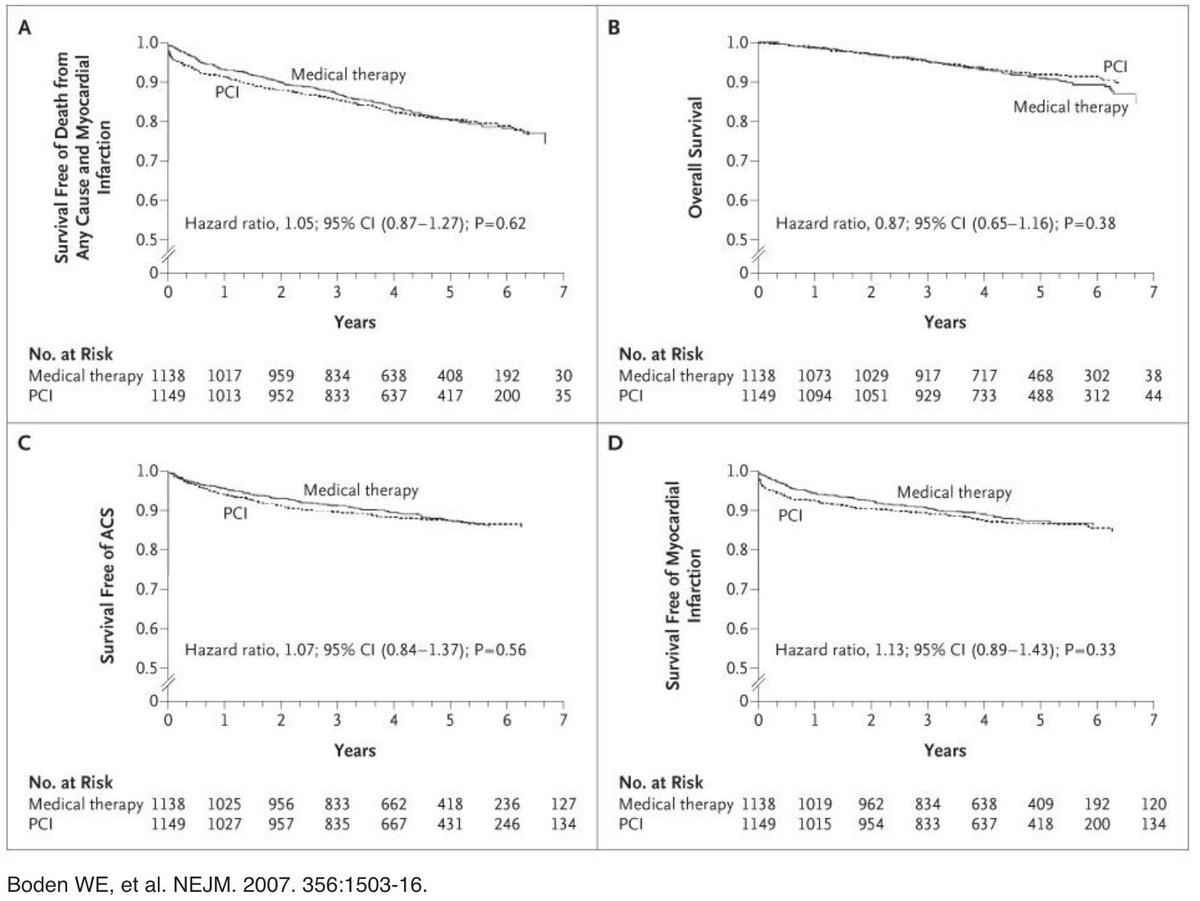
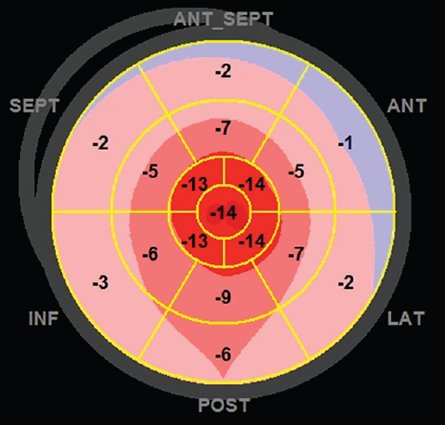
1/10 “To PCI, or Not to PCI, That is the Question” Will Shakespeare, MD
#FITSurvivalGuide
*Per many contentious #cardiotwitter discussions I realize this is loaded topic but I’m going to attempt an early stage #ACCFIT overview while recognizing there is a lot of nuance.
#FITSurvivalGuide
*Per many contentious #cardiotwitter discussions I realize this is loaded topic but I’m going to attempt an early stage #ACCFIT overview while recognizing there is a lot of nuance.

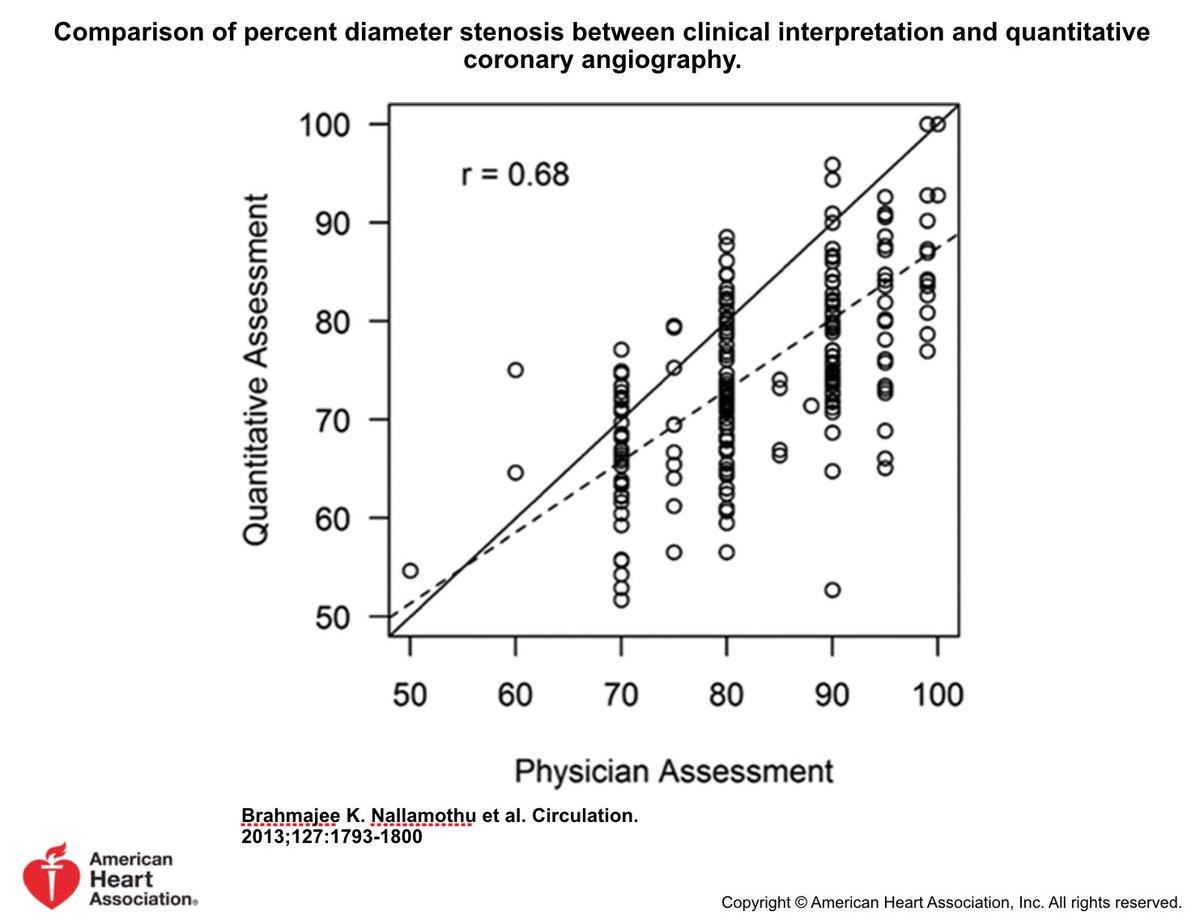
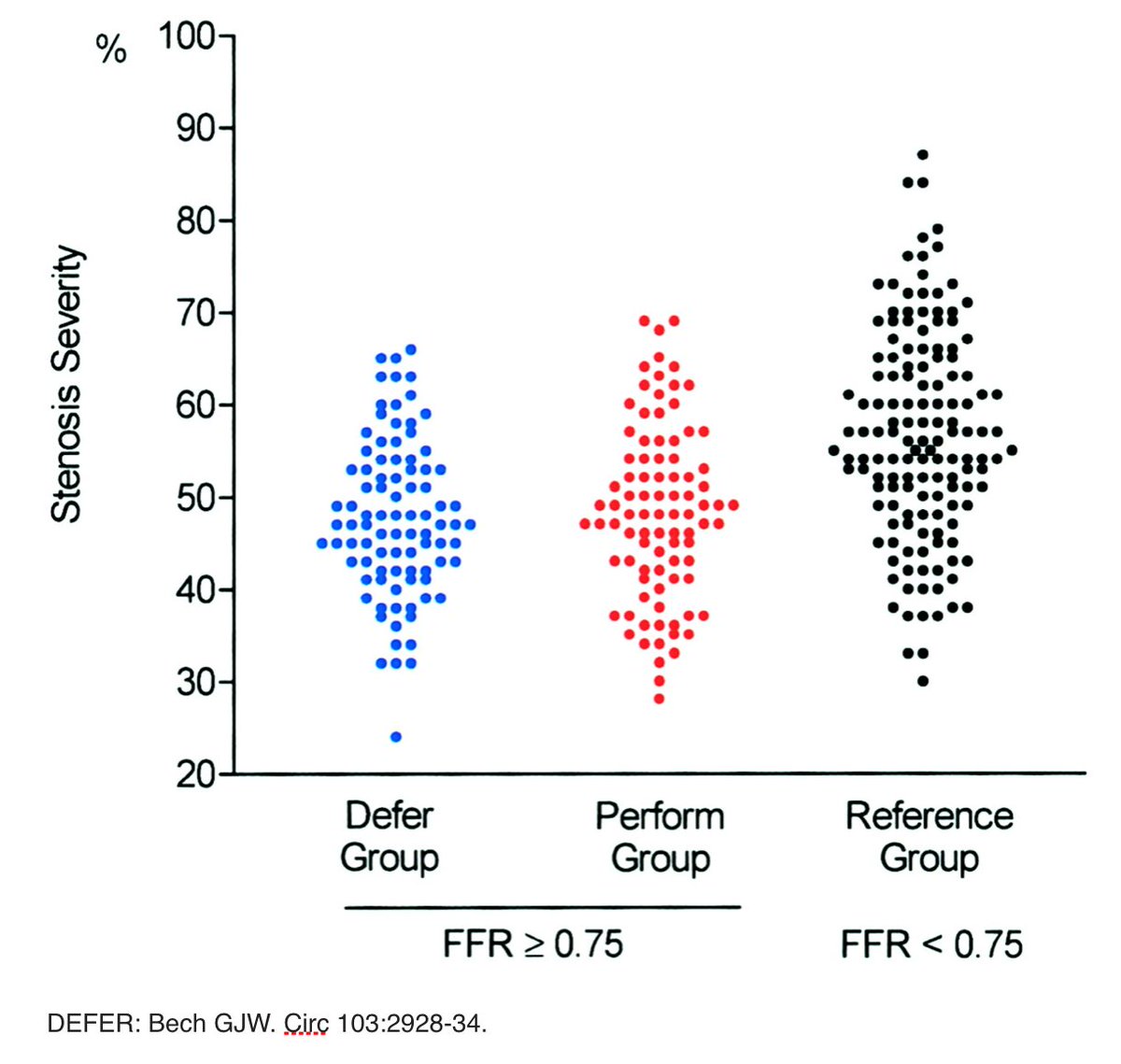
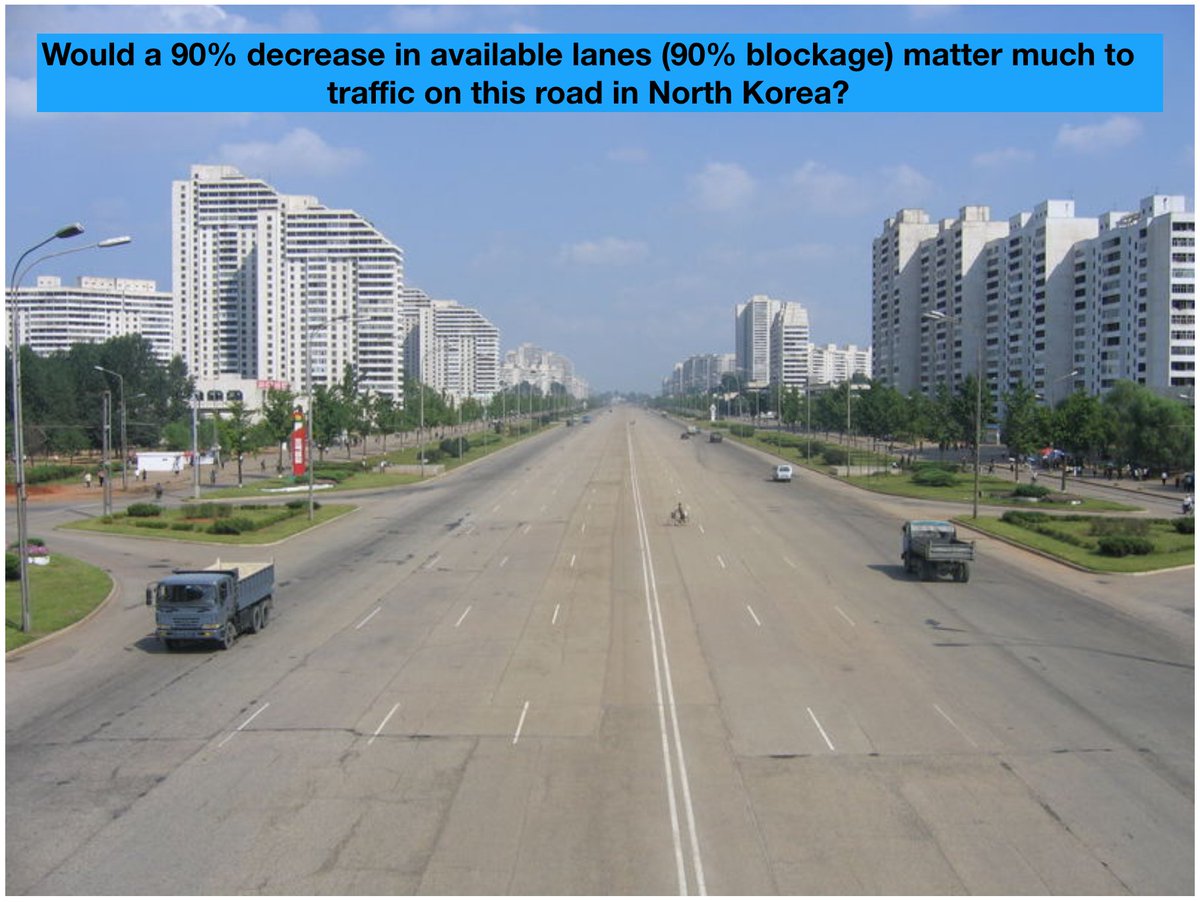
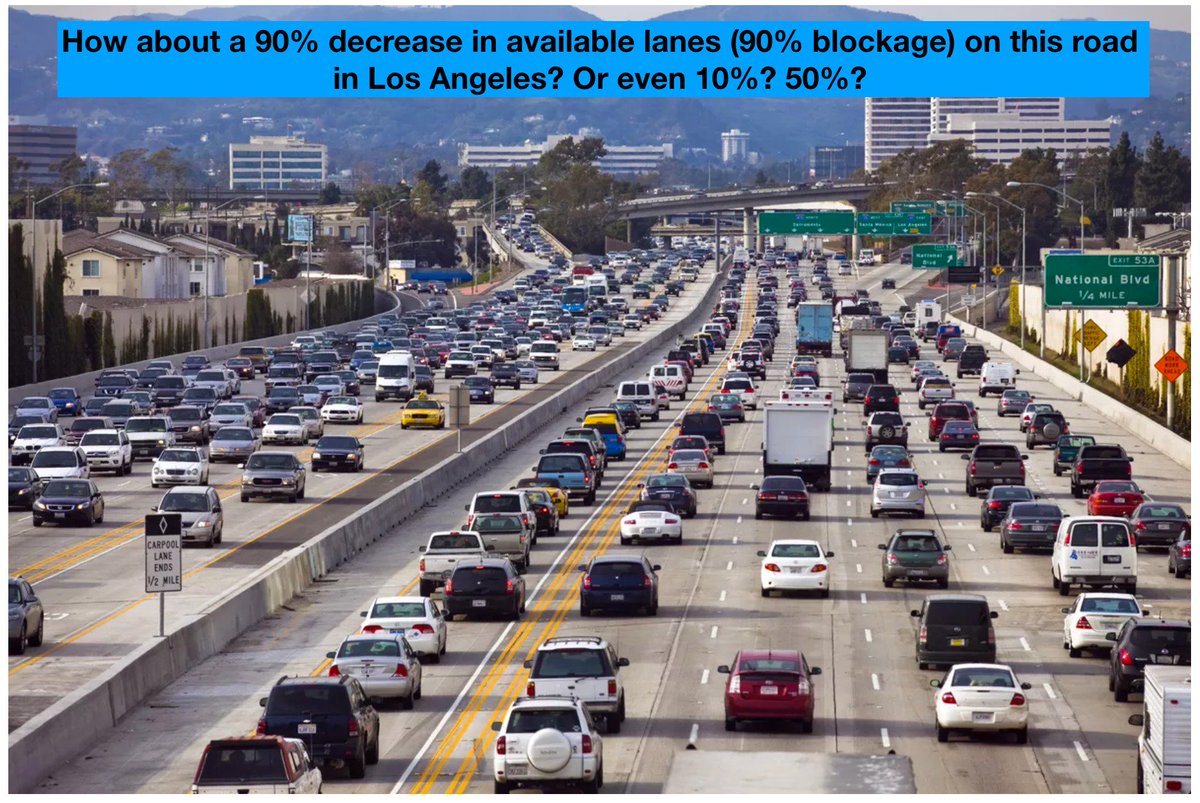
2/10 Why not “See lesion Fix lesion”?
Poor correlation between est'd visual stenosis & quantitative stenosis. And, without noninvasive ischemic data, coronary angio has limited accuracy w/ regard to identifying significance of many stenoses
*STEMI PCI already done @KhandelwalMD



Poor correlation between est'd visual stenosis & quantitative stenosis. And, without noninvasive ischemic data, coronary angio has limited accuracy w/ regard to identifying significance of many stenoses
*STEMI PCI already done @KhandelwalMD